Acquired weakness in the intensive care unit in patients with COVID-19: occurrence and associated factors
Patients with severe cases of COVID-19 may develop hypoxemic respiratory failure and acute respiratory distress syndrome, leading to the need for hospitalization in intensive care units (ICU). These patients may require organ support, particularly advanced ventilatory support, and consequently require deep sedation and neuromuscular blocking agents, some of which are known risks for the development of ICU-acquired weakness (ICUAD) in critically ill patients.
DAUCI is a common complication of critical illness, with an incidence of around 43%, which varies depending on the population studied, risk factors, timing, and methods used for diagnosis.
It is associated with increased mortality, a need for prolonged mechanical ventilation (MV), and a longer hospital stay.
Aim
The primary objective of this study was to identify the occurrence and factors associated with intensive care unit acquired weakness (ICUAD) in patients with COVID-19.
Secondarily, we monitored the evolution of muscle strength and mobility between patients with DAUCI and patients without DAUCI and the association of these variables with hospital stay, mechanical ventilation (MV) and other clinical variables.
Methods
In this prospective observational study, muscle strength and mobility of patients admitted to the ICU for > 72 h with COVID-19 were assessed at 3 time points: when they were weaned from ventilatory support, when they were discharged from the ICU and when they were discharged from the hospital. Risk factors for ICUAW were monitored.
Results
The occurrences of DAUCI in the 3 times evaluated among the 75 patients included were 52%, 38% and 13%. ICU stay (29.5 [16.3-42.5] vs. 11 [6.5-16] days; p ≤ 0.001), hospital stay (43.5 [22.8-55.3] vs 16 [12.5-24] days; p ≤ 0.001) and time on MV (25.5 [13.8-41.3] vs 10 [5-22.5] days; p ≤ 0.001) were higher in patients with DAUCI.
Muscle strength and mobility were lower at all times evaluated in patients with DAUCI ( p < 0.05).
Bed rest time for all patients (relative risk = 1.14; 95% CI = 1.02–1.28; P = 0.03 per week) and corticosteroid use (relative risk = 1.01; CI 95% = 1.00–1.03, P = .01 per day) for those requiring MV were factors independently associated with DAUCI.
Muscle strength was found to have a positive correlation with mobility and a negative correlation with ICU and hospital length of stay and time on MV.
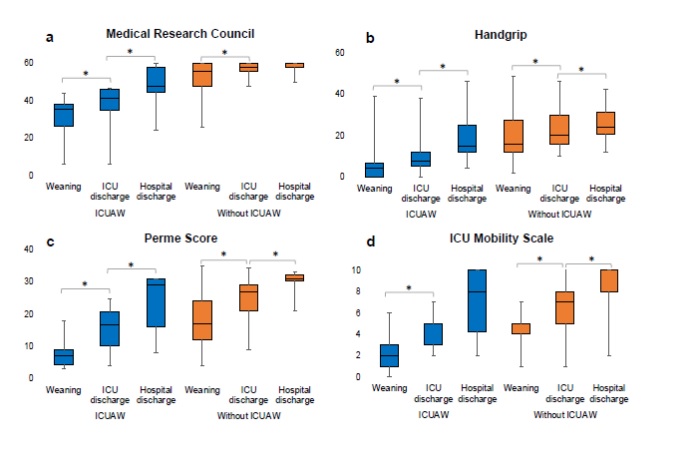
Evolution of muscle strength and mobility of subgroups of awake patients, discharged from the intensive care unit (ICU), and discharged from the hospital. The Friedman test was used to compare variables over time. ICUAW = ICU acquired weakness. *p < 0.05.
Conclusions
A high incidence of DAUCI was observed in COVID-19 patients upon awakening in the ICU, with a reduction during the hospital stay. Patients with DAUCI had longer ICU stays and the hospital used more invasive ventilatory support for longer periods, and also had difficulty weaning from MV.
These patients had lower levels of muscle strength and mobility at hospital discharge. Finally, the time of bed rest for all patients and the time of corticosteroid use for those who required IMV were factors independently associated with DAUCI in critically ill patients with COVID.
Discussion
DAUCI is a common complication in patients who are in critical condition with COVID19 and admitted to the ICU. Patients with DAUCI had longer ICU stays, hospital stays, and time on MV, received more physical therapy sessions, and had lower levels of strength and mobility upon awakening, ICU discharge, and hospital discharge.
Various clinical variables to which critically ill patients were exposed were associated with DAUCI, but the time of bed rest for all patients and the time of corticosteroid use for those who required IMV were factors independently associated with the DAUCI.
This study showed that the occurrence of DAUCI was 52.0% when patients were awakened for weaning, decreasing throughout hospitalization, 38.0% at discharge from the ICU and 13.0% at hospital discharge.
Final message
|
















