Key points Ask What is the prevalence of coronary plaque and is it associated with rates of cardiovascular events in patients with severely elevated low-density lipoprotein cholesterol (LDL-C) levels (≥190 mg/dL) who are universally considered high risk? ? ? Findings In this cohort study of 23,143 symptomatic patients, absence of coronary artery calcium (CAC) and noncalcified plaque was a common finding among those with severely elevated LDL-C levels. Across the LDL-C spectrum, the absence of CAC was associated with low rates of atherosclerotic cardiovascular disease and death, with increasing rates in patients with higher CAC burden. Meaning These findings suggest that atherosclerosis burden, including CAC assessment, can be used to individualize treatment intensity by identifying patients who are at low risk despite having very elevated LDL-C levels. |
Importance
Atherosclerosis burden and coronary artery calcium (CAC) are associated with the risk of atherosclerotic cardiovascular disease (ASCVD) events, with the absence of plaque and CAC indicating low risk.
It is not known whether this is true in patients with elevated levels of low-density lipoprotein cholesterol (LDL-C). Specifically, a high prevalence of noncalcified plaque could indicate high risk.
Aim
To determine the prevalence of calcified and non-calcified plaque in symptomatic adults and evaluate its association with cardiovascular events across the LDL-C spectrum.
Design, environment and participants
This cohort study included symptomatic patients who underwent coronary CT angiography from January 1, 2008 to December 31, 2017, from the semi-national West Danish Heart Registry. Follow-up was completed on July 6, 2018. Data was analyzed from April 2 to December 2, 2021.
Exhibitions
Prevalence of calcified and non-calcified plaque according to LDL-C strata of less than 77, 77 to 112, 113 to 154, 155 to 189 and at least 190 mg/dL.
Coronary artery disease severity was classified using CAC scores of 0, 1 to 99, and ≥100, with higher numbers indicating greater CAC burden.
Main results and measures
Atherosclerotic cardiovascular disease events (myocardial infarction and stroke) and death.
Results
In all LDL-C groups, the absence of CAC was associated with low rates of events and death
A total of 23,143 patients with a median age of 58 (IQR, 50-65) years (12,857 [55.6%] women) were included in the analysis . During a median follow-up of 4.2 (IQR, 2.3-6.1) years, 1029 ASCVD and death events occurred.
Across all LDL-C strata, absence of CAC was a prevalent finding (ranging from 438 of 948 [46.2%] in patients with LDL-C levels of at least 190 mg/dL to 4370 of 7964 [54 .9%] in patients with LDL -C of 77 to 112 mg/dL) and associated with undetectable plaque in the majority of patients, with a range of 338 of 438 (77.2%) in those with LDL levels -C of at least 190 mg/dL to 1067 of 1204 (88.6%) in those with LDL-C levels of less than 77 mg/dL.
Across all LDL-C groups, absence of CAC was associated with low rates of ASCVD and death (6.3 [95% CI, 5.6-7.0] per 1000 person-years), with increasing rates in patients with CAC scores of 1 to 99 (11.1 [95% CI, 10.0-12.5] per 1000 person-years) and CAC scores of at least 100 (21.9 [95% CI, 10.0-12.5] per 1000 person-years). 19.9-24.4] per 1000 person-years).
Among those with CAC scores of 0, the event rate per 1000 person-years was 6.3 (95% CI, 5.6-7.0) in the general population compared with 6.9 (95% CI, 4.0-11.9) in those with LDL-C levels of at least 190 mg/dl.
Across LDL-C strata, rates were similar and low in those with CAC scores of 0, regardless of whether they had no plaque or purely noncalcified plaque.
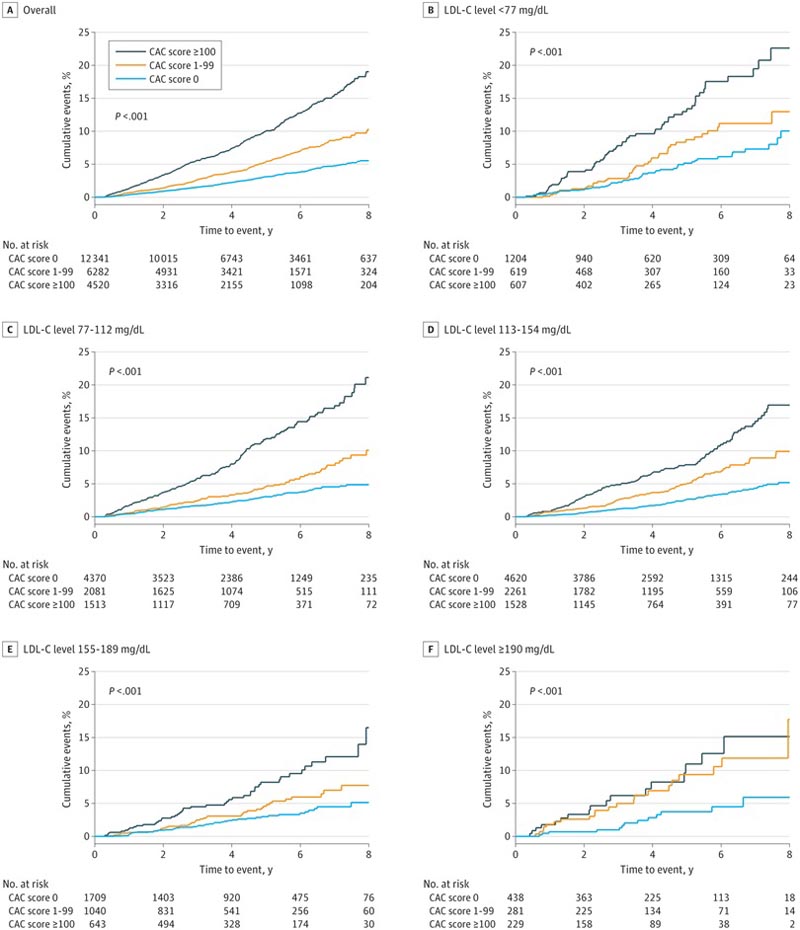
Cumulative incidence of cardiovascular disease and death stratified by coronary artery calcium (CAC) load and low-density lipoprotein cholesterol (LDL-C) levels
Conclusions and relevance
The findings of this cohort study suggest that in symptomatic patients with severely elevated LDL-C levels of at least 190 mg/dL who are universally considered high risk according to the guidelines, the absence of calcified and noncalcified plaque on CT Coronary angiography was associated with a low risk of ASCVD events.
These results further suggest that atherosclerosis burden, including CAC, can be used to individualize treatment intensity in patients with very elevated LDL-C levels.
Discussion
To our knowledge, this study includes the largest published cohort to date of patients with LDL-C levels of at least 190 mg/dL. Four key points emerge from our analyzes.
- First, atherosclerotic burden is heterogeneous across the spectrum of LDL-C levels and risk is consistently associated with plaque burden.
- Secondly, we observed absence of plaque in 46.2% of patients with LDL-C levels of at least 190 mg/dl. This proportion was similar to that of patients with lower LDL-C levels.
- Third, the absence of CCTA-proven CAC indicated no detectable plaque in 86.8% of patients, including those with LDL-C levels greater than 190 mg/dL. However, the prevalence of noncalcified plaque increased with higher LDL-C levels.
- Fourth, the absence of plaque and CAC was associated with low event rates across the LDL-C spectrum, even when non-obstructive non-calcified plaques were present. Notably, however, when noncalcified obstructive coronary artery disease was present, event rates were high, demonstrating that CAC scores of 0 miss a small proportion of high-risk individuals.
Taken together, our results support the use of CCTA results for risk stratification (including risk elimination) of symptomatic patients with high LDL-C levels. This is important because these individuals are universally considered to be at high risk with very low LDL-C goals that can only be achieved through statin treatment in combination with novel lipid-lowering therapies. Among the large proportion of patients with LDL-C levels of at least 190 mg/dL who do not have atherosclerotic plaque, the net benefit of such intensive treatment is questionable.
Patients with very high LDL-C levels (≥190 mg/dL) suggesting possible clinical familial hypercholesterolemia are currently considered high risk, with strong recommendations for lifelong therapy to lower lipid levels in US guidelines and European. However, the risk is known to be heterogeneous. Even in untreated patients with genetically verified familial hypercholesterolemia, many do not develop clinical events. Furthermore, within the same family, clinical penetrance differs markedly.
These findings demonstrate that several additional factors beyond elevated LDL-C levels affect atherogenesis in the individual patient, even though LDL-C level is the pathophysiological causative agent in atherogenesis. This principle is supported by the observation that the risk of ASCVD in patients with familial hypercholesterolemia is modified by other known risk factors beyond LDL-C levels.
Therefore, the theoretical advantage of using coronary artery disease severity information from CCTA in patients with high LDL-C is its ability to provide information on lifetime exposure to known and unknown risk modifiers. as well as the susceptibility to developing atherosclerosis in individual patients.
Viewed in that context, our study provides important information. Our data show that the absence of atherosclerotic plaque and CAC in symptomatic middle-aged patients with elevated LDL-C levels (≥190 mg/dL) is a common finding associated with low risk . Even if nonobstructive, noncalcified plaque was present, the absence of CAC was associated with low event rates. However, in individuals with noncalcific obstructive coronary artery disease, the event rate was substantially higher.
Therefore, if there is no obstructive coronary artery disease in the CCTA finding, simple CAC quantification can identify patients at low risk for ASCVD despite high LDL-C concentrations, without the need for more complex quantification. of non-calcified plaque load.
This has important clinical implications because it suggests that the allocation of adjunctive therapies to lower lipid levels, such as proprotein convertase subtilisin/kexin type 9 inhibitors, in patients with high LDL-C levels could be informed by the severity of the disease. Coronary artery disease. This information would allow the allocation of expensive long-term therapies to those patients with severe hypercholesterolemia most likely to benefit, while such therapies could be avoided in patients with limited absolute benefit.
That said, the median follow-up in our study was relatively short, 4.2 years . Because 22.8% of patients with LDL-C levels of at least 190 mg/dL had detectable plaque despite having CAC scores of 0, the results should not be used to discontinue long-term preventive therapy with statins, especially in younger people. Therefore, the results can mainly be used to avoid additional expensive and novel therapies to lower lipid levels and therefore achieve goals of very low LDL-C levels in those patients with CAC scores of 0 who would obtain a limited absolute benefit.















