what you need to know There is variation in the thresholds for diagnosing heart failure with normal ejection fraction. Treatment of heart failure with normal ejection fraction does not improve survival: however, it offers symptom relief with diuretics and treatment of hypertension and other comorbidities. More research is needed to characterize normal echocardiography in the heart during aging and to better understand the natural history of heart failure with normal ejection fraction. |
There is a lot of uncertainty surrounding heart failure with normal ejection fraction, based on its diagnosis; There are no clinical characteristics that differentiate it from heart failure with a reduced ejection fraction. 1 2
In echocardiography, the filling capacity of the left ventricle can at best only be measured indirectly. Estimates of the prevalence of heart failure with normal ejection fraction and its prognosis vary. There is doubt about the clinical relevance of the diagnosis of heart failure with normal ejection fraction due to the absence of a treatment that to date has substantially improved the prognosis. Management focuses on symptom reduction and blood pressure control. 1 2
Our preferred name is heart failure with normal ejection fraction. However, the term is used interchangeably with "preserved ejection fraction" or diastolic heart failure. These seem less accurate because "preserved" suggests prior measurement of the patient’s ejection fraction before the development of symptoms, which is not generally the case. "Diastolic" heart failure implies that systolic function is not affected, which is incorrect.
What is the evidence of uncertainty?
How is heart failure with normal ejection fraction diagnosed?
A diagnosis of heart failure requires a combination of clinical findings such as dyspnea, fatigue, and ankle edema, along with a structural or functional abnormality of the heart that affects its pump capacity on echocardiogram. 1 This alteration is usually caused by reduced left ventricular contraction, measured as a reduced ejection fraction. Reduced ejection fraction is almost always accompanied by impaired left ventricular filling, but in some patients the latter is reduced (filling capacity) while the ejection fraction is normal, this is heart failure with normal ejection fraction.
Heart failure with reduced ejection fraction is better understood: it usually develops after a myocardial infarction, when the results of myocyte loss are dilation of the left ventricle and decreased contraction. 3
Heart failure with normal ejection fraction often develops after many years of hypertension3 due to compensatory left ventricular hypertrophy leading to myocardial stiffness, with reduced filling capacity and with a small or even normal sized left ventricle. This leaves a ventricle with an ejection fraction in the normal range, but a reduced ejection volume. Patients with heart failure with normal ejection fraction may have bothersome symptoms during exercise. 3
Figure 1
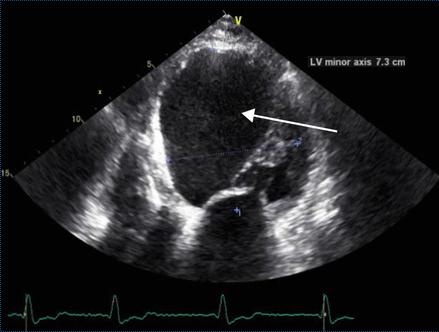
Figure 1 Echocardiogram of an elderly man with previous myocardial infarction and heart failure with reduced ejection fraction. The left ventricle is dilated (upper limit of normal for minor axis is 5.5 cm) and globular (arrow). The left ventricular ejection fraction was 24%.
Misdiagnosis of mild illness is problematic
In the early stages, heart failure with normal ejection fraction causes difficulty breathing (dyspnea: a key symptom of heart failure) that can be confused with chronic obstructive pulmonary disease (COPD), obesity, or physical deconditioning. 1 4
Fluid overload may be absent, particularly in patients receiving diuretics for hypertension. This may lead to failure to diagnose heart failure with normal ejection fraction. On the other hand, age-related dyspnea is quite common, which can lead to overdiagnosis of this condition. 5 6 7
Debate on cut-off levels for natriuretic peptides suggestive of heart failure
In the United Kingdom guidelines recommend that the diagnosis of heart failure be ruled out in patients in primary care with levels of B-type natriuretic peptide (BNP) below 100 ng/L or proBNP below 400 ng/L.2 Although a proBNP below 400 ng/L has a high negative predictive value (approximately 97%), some of the people with low levels will have heart failure with normal ejection fraction. 8
Natriuretic peptides are produced by myocytes in response to increased wall tension, which is generally lower in heart failure with normal ejection fraction than in heart failure with reduced ejection fraction, according to Laplace’s law. , since the diameter of the ventricle is smaller and the wall thickness is greater. Therefore natriuretic peptide levels are lower in heart failure with normal ejection fraction than in heart failure with reduced ejection fraction and may even be normal. 9
Lowering the baseline natriuretic peptide threshold would result in further echocardiography testing. For example, based on a prospective cohort study, lowering the cutoffs to 35 ng/L for BNP and 125 ng/L for proBNP would result in a negative predictive value of more than 99%, but at cost of many more echocardiograms. 8
Variation in cut-off levels in echocardiography
The description and cut-off points of ventricular function abnormalities in heart failure with normal ejection fraction are defined by expert consensus. Includes
(a) normal ejection fraction
(b) left atrial dilation
(c) increased left ventricular mass or wall thickness
(d) elevation of left ventricular filling pressures. 1 10
The European Society of Cardiology (ESC) and the National Institute for Health and Care Excellence (NICE) define the cut-off point for a "normal" ejection fraction as 50%, 1 2 but others suggest 45%. . There is some support for introducing an intermediate category with an ejection fraction of 40-50%. 4 11 Assessment of diastolic function in patients with atrial fibrillation is particularly difficult.
Figure 2
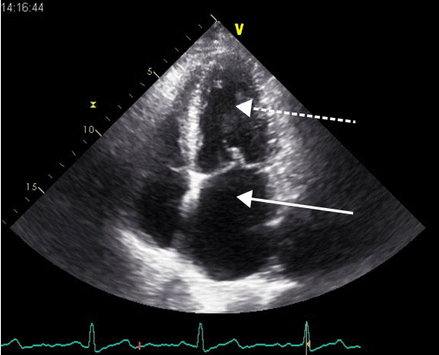
Figure 2 Echocardiogram of an older man with dyspnea. The diagnosis of heart failure with normal ejection fraction is made based on the combination of symptoms, an elevated level of N-terminal B-type natriuretic peptide (NT-proBNP), and a dilated left atrium (white arrow). Note that the left atrium is similar in size to the left ventricle (dashed arrow). The left ventricular ejection fraction was 62%.
What is the prevalence of heart failure with normal ejection fraction?
There is uncertainty about the prevalence of heart failure in the general adult population, with reported rates of 1% to 4%. 12 13 The prevalence and type of heart failure may vary depending on the population sampled. Reports based primarily on retrospective data in hospitalized patients 14 15 suggest that about 50% of patients with heart failure have a normal ejection fraction and 50% have reduced ejection fraction, with a trend over time toward an increase in heart failure with normal ejection fraction.
Prevalence data among the population of community-dwelling adults aged 65 years with heart failure found that about 75% had a normal ejection fraction and 25% had a reduced ejection fraction. 16
What is the etiology?
There is general consensus that long-standing hypertension is the most common precursor to heart failure with normal ejection fraction; As major arteries harden, they reflect the systolic pressure wave rather than absorbing it, contributing to left ventricular pressure overload.3
However, there is debate about whether other comorbidities are the cause of heart failure with normal ejection fraction or its consequences.3 17 Heart failure with normal ejection fraction may develop over many years in response to obesity. , hyperlipidemia, type 2 diabetes , COPD, and chronic kidney disease. 3 These conditions are associated with low-grade systemic inflammation and can cause coronary microvascular endothelial dysfunction, triggering hypertrophy as well as interstitial fibrosis. 3
Uncertainty is important for patients: if these (or other) comorbidities cause heart failure with normal ejection fraction, then they should be managed intensively before the disease appears.
What is the prognosis?
The prognosis of patients with heart failure with normal ejection fraction depends on the severity of the disease. About one in 10 will have died five years after diagnosis, rising to about one in three of cases first detected during hospitalization. 18 19 For comparison, the five-year mortality from colon cancer is about one in three.
In the long term, an observational study found lower cardiovascular mortality in patients with heart failure with normal ejection fraction compared with heart failure with reduced ejection fraction (adjusted hazard ratio 0.79 (95% confidence interval 0.67 to 0.95). There were no differences in non-cardiovascular mortality. 15
An analysis of individual patient data from 31 studies (both hospital-based, observational studies, and randomized clinical trials) found an adjusted hazard ratio for all-cause mortality of 0.68 (0.64 to 0.71) for heart failure. heart failure with normal ejection fraction compared to heart failure with reduced ejection fraction. 18
Among community-dwelling patients older than 60 years with type 2 diabetes, all-cause mortality in newly detected cases of heart failure with normal ejection fraction was also lower than in cases of heart failure with normal ejection fraction. reduced ejection rate (1.51 v 3.31 per 100 person-years). 19
How should it be managed?
There is no therapy that significantly improves survival or prevents hospitalizations in patients with heart failure with normal ejection fraction. 1 2 Four large randomized controlled trials of drugs that counteract the renin-angiotensin system (RAS) showed no clear impact on survival. 20 21 22 23 However, the trials’ inclusion criteria meant that some healthy people could have been included because no clear criteria for echocardiographic diastolic dysfunction were applied, and natriuretic peptides were not used as an inclusion criterion. 20 21 22 23
The quality of life of heart failure patients with normal ejection fraction can be improved through exercise, according to a recent meta-analysis of six randomized controlled trials (276 patients combined), but its validity is questionable given the small sample analyzed. 24
What should we do in light of uncertainty?
Assessment
|
Management
Offer people with a confirmed diagnosis of heart failure with normal ejection fraction diuretics titrated according to symptoms (treatment based on consensus opinion).
Hypertension and other concomitant diseases must be managed appropriately. Consider encouraging exercise after reassuring patients that their practice is safe.
The future: there is numerous research underway on different topics
We searched http://clinicaltrials.gov databases and found several ongoing trials evaluating different drugs targeting different potential mechanisms in heart failure with normal ejection fraction:
- Inhibition of myocardial fibrosis
Interleukin-1 blockade
- Vasodilation
Blockade of the renin-angiotensin system, together with inhibition of neprilysin with valsartan sacubitril
- We also found trials that evaluated:
Exercise training
Renal denervation
Optimal management of comorbidities
- Other research explores
the normal aging process of the healthy heart, and the differentiation of heart failure with normal ejection fraction from normal aging.
Refined diagnostic criteria for heart failure with normal ejection fraction.
Recommendations for future research
- Define the normal ranges of echocardiographic variables at different ages in a large and representative sample of the community living in older people.
- Develop robust diagnostic criteria for the definition of heart failure with normal ejection fraction.
- To apply diagnostic criteria for community-dwelling adults to define the true prevalence and prognosis of heart failure with normal ejection fraction.
- Apply diagnostic criteria for participants in clinical trials evaluating pharmacological treatment of heart failure with normal ejection fraction.
- To determine the mechanisms underlying the development of heart failure with normal ejection fraction. The discovery of the pathobiology can reveal avenues for treatment.
- Design randomized controlled trials of heart failure patients with normal ejection fraction with robust inclusion criteria: to investigate appropriate drugs, to compare interventions with usual care and placebo, and to assess mortality and hospitalization outcomes.