Goals
Analyzing the evidence regarding the health burden of chronic venous insufficiency (CVI), its clinical determinants and impact on outcome is scarce.
Methods and results
Systematic phenotyping of CVI according to the established CEAP ( Clinical-Etiologic-Anatomic-Pathophysiologic ) classification was performed on 12,423 participants (age range: 40-80 years) of the Gutenberg Health Study from April 2012 to April 2017.
Prevalence was calculated according to age. and specifically by sex. Multivariable Poisson regression models were calculated to evaluate the relationship of CVI with cardiovascular comorbidities. Survival analyzes were performed to evaluate the risk of death associated with CVI.
Replication of the findings was performed in an independent cohort study (MyoVasc, NCT04064450). The prevalence of telangiectasia/reticularis, varicose veins, and CVI was 36.5% [95% confidence interval (CI), 35.6%-37.4%], 13.3% [12.6%-13 .9%] and 40.8% [39.9% -41.7%], respectively.
Age, female sex, high blood pressure, obesity, smoking, and clinically manifest cardiovascular disease were identified as clinical determinants of CVI.
Higher CEAP classes were associated with a higher 10-year predicted risk of incident cardiovascular disease in cardiovascular disease-free individuals (n = 9923).
During a mean follow-up of 6.4 ± 1.6 years , CVI was a strong predictor of death from any cause, regardless of concomitant clinical profile and medication [hazard ratio (HR) 1.46 (95% CI). : 1.19-1.79), P = 0. 0003].
The association of CVI with an increased risk of death from any cause was externally validated in the MyoVasc cohort [HR 1.51 (95% CI: 1.11–2.05), P = 0.009].
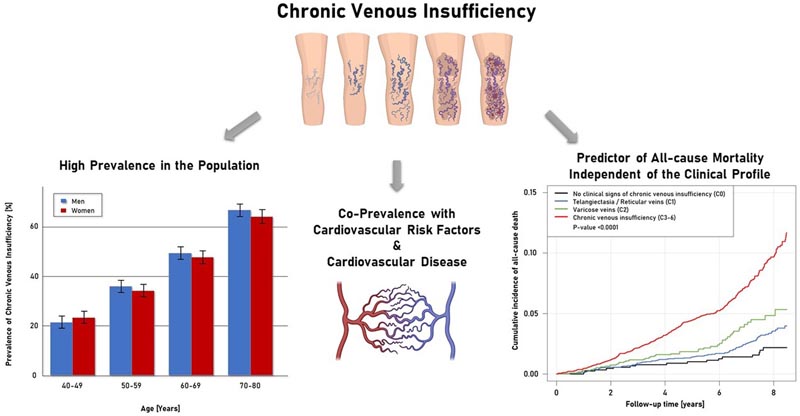
Chronic venous insufficiency is highly prevalent in the general population and is associated with arterial cardiovascular disease and an increased risk of all-cause mortality.
Conclusion
|
Comments
A window to the heart
Chronic venous disease has a high global prevalence, with various manifestations ranging from telangiectasias to varicose veins and, in advanced cases, ulcerations.
The underlying pathophysiology involves venous hypertension in the legs induced by several potential factors, including venous valve dysfunction leading to retrograde blood flow, calf muscle pump dysfunction, and systemic hemodynamic changes including obesity and right heart failure.
The diagnosis of chronic venous disease is based on the typical features of the physical examination that are included in the Clinical, Etiological, Anatomical, Physiopathological (CEAP) classification system: telangiectasia or reticular veins, varicose veins, edema, pigmentation or lipodermatosclerosis and ulceration.
Treatment includes compression therapy for all and interventional therapy in selected patients . Previous studies have explored risk factors for chronic venous disease including age, obesity, female sex, smoking, family history, and previous venous thrombosis.
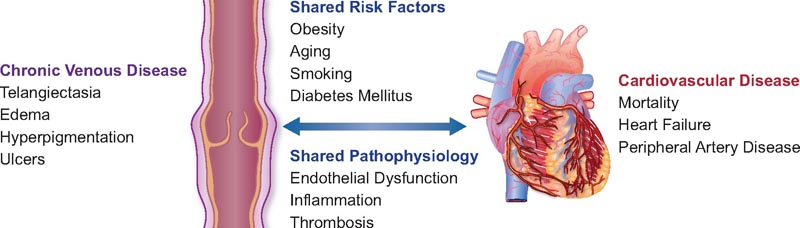
The presence of shared risk factors for chronic venous disease and cardiovascular disease prompted the epidemiological investigation of Prochaska and his colleagues from the Gutenberg Heart Study.
In 12,423 adult participants in the population-based cohort study, researchers classified chronic venous disease using the CEAP system by evaluating the appearance of the lower extremities on physical examination and digital photographs (graded by independent investigators) and the self-reported venous symptoms.
Cross-sectional analysis at baseline confirmed a high prevalence of any chronic venous disease (36.5%). Lower extremity edema had the highest prevalence (30%) and ulceration the lowest prevalence . Women had a greater burden of chronic venous disease compared to men, and the disease shifted toward greater severity with advancing age.
In addition to the previously reported association of obesity, hypertension, and smoking with chronic venous disease, the current study reports higher rates of estimated cardiovascular risk based on the Framingham risk score with increasing severity of chronic venous disease.
Participants with chronic venous disease had an existing burden of cardiovascular disease, including prior venous thromboembolism, a known inducer of chronic venous disease, but also peripheral arterial disease. Patients with established heart failure in the MyoVasc cohort had a high prevalence of advanced chronic venous disease (C4-C6) of 14%.
Intersections of chronic venous disease and cardiovascular disease.
The vascular endothelium regulates arterial and venous homeostasis, and cardiovascular risk factors lead to systemic endothelial dysfunction.
Venous endothelial cells show reduced nitric oxide signaling in patients with diabetes, obesity, and smoking. Veins harvested from patients with chronic venous disease show increased oxidative stress, increased inflammation, and altered endothelial function.
Biomarkers of thrombosis and inflammation are also present. higher in lower extremity samples from patients with chronic venous disease, suggesting common factors of venous and arterial injury.
Recent genetic studies of varicose veins have identified pathways of vascular development that overlap with the genetics of venous thrombosis. The genetic epidemiology of venous thrombosis demonstrates extensive intersections with arterial disease, including lipids and plasminogen activator inhibitor type 1 (PAI-1). It will be important to evaluate whether the genetics of the chronic venous disease spectrum identify pathways shared with heart failure or arterial diseases.
Evaluation of 6-year follow-up data demonstrated that chronic venous disease predicts all-cause mortality in models adjusting for cardiovascular risk factors and persists in analyzes that exclude participants with prevalent cardiovascular disease at 6 years. start of the study. The predictive value of chronic venous disease was also demonstrated in the MyoVasc cohort of patients with established heart failure.
While not the first study to connect venous disease to cardiovascular events, the current study adds a comprehensive assessment of the spectrum of chronic venous disease, indicating that progression in severity by CEAP class portends increased risk of mortality. One interpretation of the elevated risk of mortality with chronic venous disease includes the impact of shared risk factors that negatively influence the heart and drive venous hypertension.
Since leg edema was the most common manifestation of chronic venous disease, it is also possible that the increased risk reflects edema as an early sign of undetected heart failure.
This possibility is supported by the stronger association of venous insufficiency with edema. and skin changes with prevalence of cardiovascular disease and risk of mortality compared to varicose veins. Still, the study’s findings indicate that a simple physical examination to identify chronic venous disease has potential clinical value in adults with or without established cardiovascular disease.
The American Heart Association conducted the “Kick Your Socks Off” public awareness campaign with physicians to identify the presence of peripheral artery disease. The study by Prochaska et al. It provides another reason to examine our patients’ legs for signs of chronic venous disease as a window to the heart .
In patients without established cardiovascular disease and those with heart failure, observation of the presence of varicose veins, edema, skin changes, and ulcers provides a simple clinical marker of excessive risk .
















