Highlights In this study, the authors used a modified Delphi method to obtain expert consensus on the definition and severity categories of chronic obstructive pulmonary disease (COPD) exacerbation. The expert panel proposed incorporating measurable clinical and laboratory values, including dyspnea severity, oxygen saturation, respiratory rate, heart rate, C-reactive protein, and arterial blood gas. This updated definition, called the "Rome proposal" , will help standardize the care of patients diagnosed with an acute exacerbation of COPD and homogenize research. |
Where we are?
Scientific knowledge on the topic:
Precise and practical definitions for acute medical events are needed if physicians are to effectively diagnose and treat patients, provide prognostic information, and implement precision medicine. The current definition of exacerbation of chronic obstructive pulmonary disease (COPD) is subjective and based solely on worsening respiratory symptoms. Additionally, severity is classified post hoc by the healthcare resource used to treat the event. These deficiencies support the need to revise the definition of ECOPD.
What this study adds to the field:
Rome’s proposal for an updated definition of ECOPD addresses many of the shortcomings of older definitions. Based on an extensive review of the literature and using the Delphi methodology, it specifies the time period within which worsening symptoms define an ECOPD.
Secondly, to the subjective worsening of symptoms it adds a series of clinical variables that are objectively measurable and easily available : dyspnea, oxygen saturation, respiratory rate, heart rate, C-reactive protein and, if necessary, arterial blood gases.
Third, based on agreed upon thresholds, it integrates these variables into three mutually exclusive severity categories that can be used to classify the severity of the exacerbation at initial patient contact. This proposal aims to facilitate and improve clinical care, research and planning of health services.
The current definition of exacerbation of chronic obstructive pulmonary disease (COPD) is based solely on worsening respiratory symptoms, with severity classified post hoc by the healthcare resource used to treat the event, which can vary between professionals and systems. sanitary.
These deficiencies support the need to revise the ECOPD definition and severity classification to one that is useful at the time of patient contact. To achieve this, an expert panel used a modified Delphi method of five rounds of questions generated by a comprehensive literature review, complemented by virtual discussions. For the 80 questions identified, the level of agreement was rated using a Likert scale from 0 (strongly disagree) to 9 (strongly agree). Consensus was defined a priori as a median score ≥7 (strong agreement).
The ECOPD conceptual model and proposed definition
Current evidence indicates that an ECOPD is characterized by an acute burst of airway inflammation due to bacteria, viruses, environmental pollutants, or other stimuli (Figure 1). This has been documented by carefully conducted studies in the outpatient and hospital settings, with many studies showing that the inflammatory process can spread systemically.
This inflammatory burst, along with worsening existing airflow limitation, increases the work of breathing in patients with limited respiratory reserve.
A vicious cycle of increased airway resistance and tachypnea leads to gas trapping in the lungs, respiratory muscle dysfunction, worsening dyspnea, and ventilation-perfusion mismatch manifesting as arterial hypoxemia with or without hypercapnia . In some patients, ventilatory demand exceeds reserve, leading to ventilatory insufficiency, hypercapnia, and respiratory acidosis that, if untreated, can cause death.
Diagnostic method
1) These events can be life-threatening and require appropriate evaluation and treatment.
2) Complete a thorough clinical evaluation for evidence of COPD and possible respiratory and non-respiratory comorbidities, including consideration of alternative causes for the patient’s symptoms and signs; mainly pneumonia, heart failure and pulmonary embolism.
3) Evaluate:
a) Symptoms; severity of dyspnea using VAS and documentation of the presence of cough.
b) Signs (tachypnea, tachycardia), volume and color of sputum and respiratory difficulty (use of accessory muscles).
4) Assess severity by appropriate additional investigations such as: pulse oximetry, laboratory evaluation, CRP and/or arterial blood gases.
5) Establish the cause of the event (virus, bacterial, environmental, other).
Causes, pathobiological mechanisms and pathophysiological consequences in a COPD exacerbation
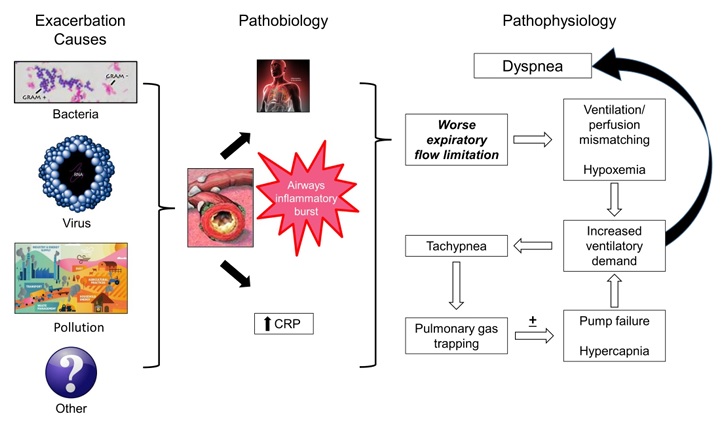
COPD, chronic obstructive pulmonary disease; VAS, visual analogue scale; CRP, C-reactive protein.
Definitions
| The proposed definition states: "In a patient with COPD, an exacerbation is an event characterized by dyspnea and/or cough and sputum that worsens in ≤14 days, which may be accompanied by tachypnea and/or tachycardia, often associated with local increase and systemic inflammation caused by respiratory tract infection, pollution, or other damage to the respiratory tract.” |
ECOPD severity classification
The current classification of ECOPD severity, based on post-facto utilization of healthcare resources, is a major limitation of the current definition. Due to global variability in resources available to treat patients and local customs that affect criteria for hospital visits and admissions, there is substantial variability in outcomes reported by the ECOPD. This is of particular importance in interpreting the results of intervention studies and in planning future clinical trials.
Three categories of severity (mild, moderate or severe) were defined by integrating six clinically measurable variables :
- Intensity of dyspnea
- Oxygen saturation
- Breathing frequency
- Heart rate
- C-reactive protein
- If indicated, arterial blood gases.
These variables were agreed upon by consensus from a possible list of 21 that were the subject of an exhaustive literature review and discussion. Of these possible variables, worsening cough and sputum deserved special attention. During ECOPD, cough and increased sputum or color change may occur and, in a proportion of cases, it may be the most relevant symptom or sign; however, its intensity has not been correctly measured, making it difficult to include in the severity classification of ECOPD.
However, although cough and sputum remain an integral part of the definition of ECOPD, the panelists agreed that worsening dyspnea is the most relevant symptom for most patients and, since it is measurable, It is useful to classify the severity of the episode.
Hypoxemia and hypercapnia
Ventilation-perfusion imbalance (VA/Q) is the most important mechanism responsible for gas exchange abnormalities in COPD.
Since stable COPD can be associated with arterial hypoxemia with or without hypercapnia, both absolute measurements and a change in values would be useful as determinants of severity. Blood gas assessment is ideal but not available in all clinical settings, while pulse oximetry is practical and widely available, although we recognize it may be less accurate in black patients.
Decompensated hypercapnic respiratory failure is known to be associated with increased mortality that is reduced by non-invasive ventilation (NIV). Although expert societies recommend titrating supplemental oxygen during ECOPD to a SaO2 of 88 to 92% (7, 55), ECOPD studies suggest that the average reduction in SaO2 was no more than 2%.
Based on this evidence, the panel agreed that when the change from baseline is known, a mild ECOPD would be characterized by arterial oxygen saturation (SaO2) ≥92% and a change ≤3%, a moderate event would be SaO2 <92 % and/or a change > 3%, and a severe event due to acidotic hypercapnic respiratory failure , i.e. arterial partial pressure of carbon dioxide (PaCO2) > 45 mmHg and pH < 7.35.
Serum C-reactive protein
A CRP value ≥10 mg/L can help separate mild from moderate ECOPD.
Healthy subjects, smokers without COPD, and patients with stable COPD typically have CRP values <10 mg/L, with higher values within this range associated with an increased risk of hospitalization and death. Serum CRP levels increase in both viral and bacterial ECOPD, although they are usually higher in the latter, so point-of-care values can be used to guide antibiotic therapy.
In outpatients with COPD who suffer from ECOPD, CRP levels increase modestly compared to baseline values. In patients in the emergency room or admitted to the hospital, higher CRP values have been reported, ranging between 8-156 mg/L.
Although the panel recognized the lack of specificity of serum CRP as a marker of airway or lung inflammation, consensus was reached that a CRP value ≥10 mg/L can help separate mild from moderate ECOPD. .
We did not assign CRP a weight different from HR, RR or oxygen saturation. A patient could have a more severe episode defined exclusively by a combination of clinical signs without a CRP > 10 mg/L. Our proposal aims to help drive the inclusion of at least one measurable point-of-care marker, the threshold of which can be be modified over time, if this proposal is implemented and the results suggest so.
Integration of variables into a practical severity rating scale
The panelists agreed that the integration of the five easy-to-assess parameters (dyspnea, respiratory rate, heart rate, oxygen saturation and serum CRP) will be used to evaluate the severity of an ECOPD, both in the clinical evaluation of patients and in research. and clinical trials.
|
The Rome proposal for an updated definition and severity classification of ECOPD was drafted by an international panel of experts, using a framework that focused on feasibility and potential validity. Consensus was reached using a modified Delphi methodology, based on data from studies that reported objective measurements of symptoms, signs, physiological variables, and biomarkers.
The predictive value of variables classifying severity was evaluated using the potential intensity of care necessary for the treatment and stabilization of the patient. This revised definition addresses many of the shortcomings of the current definition and should better inform clinical care, research, and health services planning, but needs to be prospectively validated in appropriately designed and powered studies.
Other important tests
Panelists reviewed 16 other clinical and laboratory tests used in the diagnosis and severity classification of ECOPD. Of these, several require some comment.
Routine spirometry or any assessment of lung function cannot be reliably obtained during an ECOPD since patients are usually too ill to perform an adequate spirometry maneuver, changes from baseline are often small, and results prior to ECOPD may not be available.
The panelists also thought that the efforts made to develop accurate devices that can help monitor lung function over time would provide an important advance in our ability to integrate this variable into future improvements in this proposal.
Peripheral blood eosinophils would have potential use as a therapeutic guide, particularly with respect to systemic steroid use, but eosinophil levels have not been used for ECOPD diagnosis or severity classification.
Chest x-ray is useful in differentiating pneumonia (and other conditions that can mimic ECOPD such as pneumothorax or pleurisy) from ECOPD and is frequently obtained in patients treated in healthcare facilities, but this tool has not been used to define or classify the severity of an ECOPD.
| In conclusion , by incorporating clinical and laboratory variables measurable at the time of exacerbation, the Rome proposal for an updated definition of ECOPD could help standardize care and outcomes for both clinicians and researchers. |















