Key points
|
Long recognized as a transformative innovation, advanced imaging has come under increased scrutiny. Payments for imaging have seen disproportionate growth, and up to half of all imaging studies ordered in the United States may be unnecessary.
Reflecting this tension and despite the initiative’s intentionally broad scope, most of the Choosing Wisely campaign’s initial recommendations involved physicians. Additionally, the long-term harms of radiation exposure are gaining more recognition, given evidence of the association between doses in the range of common computed tomography (CT) scans and an increased risk of developing cancer in the future. The threefold increase in the volume of CT procedures in the United States over the past 2 decades to more than 85 million in 20112 are inconsistency in radiation dose per exam and variation in dose at the facility level of up to 13-fold.
Recommendations for the diagnostic evaluation of hematuria provide an instructive framework within which to consider the benefits, harms, and costs associated with CT. Hematuria is prevalent, and nearly 2 million Americans annually are referred to urologists for this finding.
Current guidelines emphasize a structured evaluation that includes cystoscopy and imaging to rule out urinary tract malignancy, although the threshold for referral and the recommended imaging modality remain uncertain. given the limitations in the evidence. Given the prevalence, different recommendations may result in considerable variation in population-level costs and patient burden of subsequent sequelae.
Previous cost-effectiveness analyzes have suggested that substantial incremental costs and minimal benefits are associated with replacing ultrasound with CT. Although provocative, these studies have important limitations. First, asymptomatic microscopic hematuria, the focus of these analyses, has a relatively low pretest probability of cancer.
Previous publications, including one that serves as the basis for the estimates of these other studies, have shown that almost 20% of referred patients may have a history of gross hematuria, which is associated with an order of magnitude increased risk of cancer.
Second, one study modeled renal cell carcinoma (RCC) and upper tract urothelial carcinoma (UTUC) as a composite outcome despite differences in CT and ultrasound for these diagnoses, and the other study assumed a perfect sensitivity for CT.
The authors of these studies have expressed concern about the potential harms of radiation exposure from CT scans, as noted elsewhere, real-world dose variation has not been considered. Multiphase computed tomography of the abdomen and pelvis has been associated with not only the highest mean dose, but also the widest dose range and, in turn, the highest adjusted lifetime attributable cancer risk among protocols. of common CTs.
In this context, we used microsimulation models to compare the benefits, harms, and costs associated with different guidelines for hematuria evaluation. We included patients with macroscopic and microscopic hematuria in the simulated population, considering the detection of upper tract cancers as discrete entities and taking into account CT dose variation in real-world practice.
Summary
Importance
Existing recommendations for diagnostic testing for hematuria range from uniform assessment of variable intensity to risk stratification at the patient level. Concerns have been raised not only about the costs and benefits of computed tomography (CT) but also about the potential harms of exposure to CT radiation.
Aim
To compare the benefits, harms, and costs associated with 5 guidelines for the evaluation of hematuria.
Design, environment and participants
A microsimulation model was developed to evaluate each of the following guidelines (listed in order of increasing intensity) for the initial evaluation of hematuria: Dutch, Canadian Urological Association (CUA), Kaiser Permanente (KP), Hematuria Risk Index (HRI ) and the American Urological Association (AUA).
Participants comprised a hypothetical cohort of patients (n = 100,000) with hematuria aged 35 years or older. This study was conducted from August 2017 to November 2018.
Exhibitions
According to Dutch and CUA guidelines, patients received cystoscopy and ultrasound if they were 50 years or older (Dutch) or 40 years or older (CUA). According to KP and HRI guidelines, patients received different combinations of cystoscopy, ultrasound, and CT urography or no evaluation depending on risk factors. According to AUA guidelines, all patients aged 35 years or older received cystoscopy and CT urography.
Main results and measures
Detection rates of urinary tract cancer , radiation-induced secondary cancers (from CT radiation exposure), procedural complications, false positive rates per 100,000 patients, and incremental cost per additional urinary tract cancer detected.
Results
The simulated cohort included 100,000 patients with hematuria, aged 35 years or older. A total of 3514 patients had urinary tract cancers (estimated prevalence, 3.5%; 95% CI, 3.0%-4.0%).
The AUA guidelines missed the fewest cancers (82 [2.3%]) compared to the detection rate of the HRI (116 [3.3%]) and KP guidelines (130 [3.7%] ]). However, the simulation model projected 108 (95% CI, 34-201) radiation-induced cancers according to KP guidelines, 136 (95% CI, 62-229) according to HRI guidelines, and 575 (95% CI, 184-1069) according to AUA guidelines per 100,000 patients. The CUA and Dutch guidelines missed detection of a larger number of cancers (172 [4.9%] and 251 [7.1%]), but did not have radiation-induced secondary cancers.
The AUA guidelines cost approximately twice as much as the other 4 guidelines ($939/person vs. $443/person for the Dutch guidelines), with an additional cost of $1034374 per urinary tract cancer detected compared to the AUA guidelines. HRI.
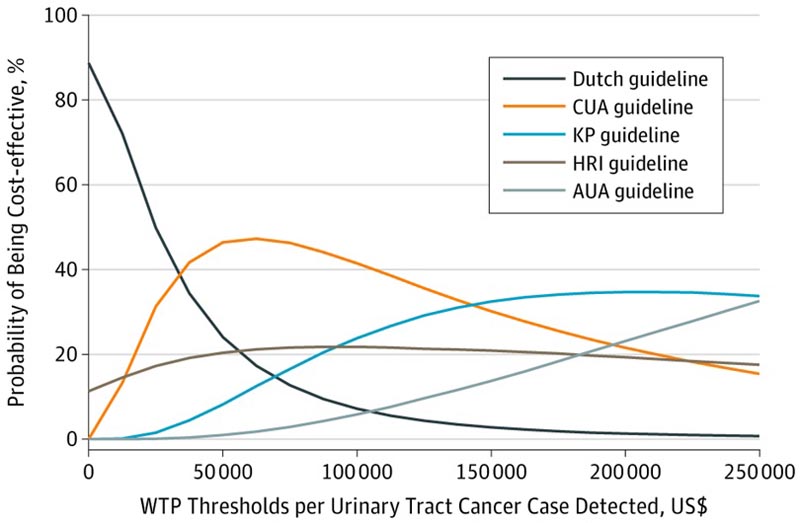
Each CEAC represents the probability that a strategy is cost-effective under different willingness-to-pay (WTP) thresholds for an additional case of hematuria-associated urinary tract cancer detected. There is no commonly accepted cost-effectiveness threshold with which to compare incremental cost-effectiveness ratios expressed as incremental cost per additional urinary tract cancer detected; therefore, a wide range of possible DAP thresholds was drawn. AUA indicates American Urological Association; CUA, Canadian Urological Association; HRI, hematuria risk index; and KP, Kaiser Permanente.
Conclusions and relevance In this simulation study, uniform CT imaging for patients with hematuria was associated with increased costs and harms from secondary cancers, procedural complications, and false positives, with only a marginal increase in cancer detection. Risk stratification can optimize the balance of benefits, harms, and costs of CT. |
Comments
Strict adherence to guidelines recommending uniform use of computed tomography (CT) to evaluate hematuria appears to cause radiation-induced cancers that erase the diagnostic advantage of CT, according to a study in JAMA Internal Medicine.
The researchers evaluated the benefits and harms of five guidelines.
- One, from the American Urological Association (AUA), recommends cystoscopy and CT urography in all cases of hematuria in patients 35 years of age and older.
- Others, for example the Dutch and Canadian guidelines, recommend cystoscopy and ultrasound (or no intervention) depending on the patient’s age and risk.
- Kaiser Permanente guidelines recommend CT only with gross hematuria.
In a theoretical sample of 100,000 patients with hematuria, the AUA detection rate was higher (98%), while the Dutch rate was lower (93%).
However, CT radiation-induced cancers amounted to 575 cases per 100,000 with the AUA approach, versus 108 with Kaiser. Furthermore, the additional cost of finding an additional cancer with the AUA approach relative to, for example, the Kaiser approach, was approaching $1 million.
The commentators note that for now, "the best available evidence suggests that uniform use of CT for the initial evaluation of microscopic hematuria is not advisable ."















