UNIVERSITY COLLEGE LONDON
Summary It is often suggested that hygiene is not compatible with microbial exposures that are necessary for the establishment of the immune system in the first years of life. However, when we look at the microbial exposures of modern humans in the context of human evolution and history, it becomes clear that while children need exposure to the microbiotas of their mothers, other family members, and the natural environment , exposure to the unnatural microbiota of the modern home is less relevant. Furthermore, any benefit from exposure to childhood infections within your family environment is superseded, at least in part, by the recently revealed nonspecific effects of vaccines. Focusing hygiene practices on key risk times and sites can maximize protection against infection and minimize any impact on essential microbial exposures. Additionally, this guidance should aim to reduce children’s direct exposure to cleaning agents because these agents likely exert TH2 adjuvant effects that trigger allergic responses to normally innocuous antigens. Finally, it is necessary to stop the flow of publications in scientific literature and the media that blame hygiene for the increase in immunoregulatory disorders. Properly targeted hygiene behavior is compatible with a healthy lifestyle that promotes exposure to essential microorganisms. |
Microorganisms found in early life populate the microbiota and provide data to expand and select lymphocyte clones and molecular signals such as some forms of endotoxins and muramic acid derivatives that drive the development of the innate and adaptive immune systems along with their mechanisms. crucial immunoregulatory control.
Defective immunoregulation is , at least in part, responsible for the increased prevalence of chronic inflammatory disorders, such as allergies, autoimmunity, and inflammatory bowel diseases that emerge as societies adopt Western lifestyles.
It has been suggested that this defective immunoregulation is attributable to distortion of microbial inputs in early life by domestic hygiene practices. However, hygiene in our homes and in everyday life is a life-saving strategy .
In this article we use the word hygiene to refer to the practices used to prevent the spread of infection. The term cleaning will be used to refer to practices used to remove dirt and to produce a surface that is visibly and aesthetically clean through the use of products containing materials such as surfactants, soaps, enzymes, oxidizing agents, acids or ammonia.
Developing targeted hygiene allows us to modify behavior so that it preserves essential microbial exposures while continuing to protect against infection. We reached this conclusion by combining an evolutionary approach with recent advances in our understanding of the roles of nonspecific effects of vaccines and a TH2 adjuvant effect of direct exposure to clearance agents.
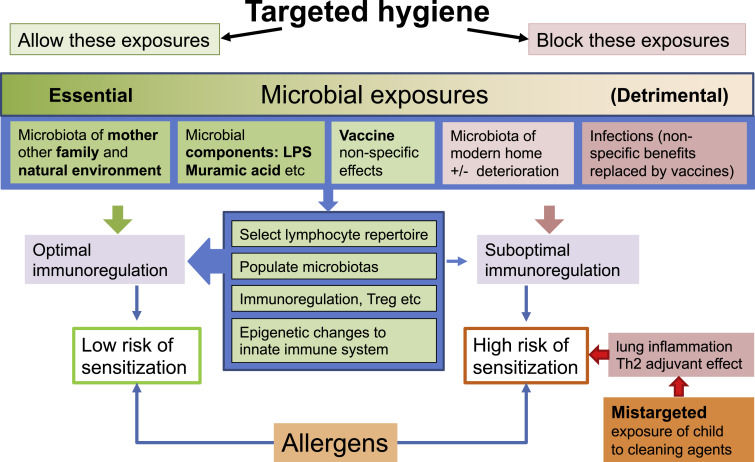
Microbial communities that hygiene should and should not target. The proper development of the immune system and its immunoregulatory mechanisms can be driven by the microbiota of the mother (and siblings) and the natural environment, complemented by the nonspecific effects of vaccines. Targeted hygiene avoids reducing these exposures and also avoids exposing the child to those cleaning agents that may have TH2 adjuvant properties (explained and mentioned in Figure 2) while reducing exposure to infections and harmful contaminants from modern homes in deterioration. Of course, there is some overlap between microbial communities.
Comments
The theory that modern society is too clean , leading to a faulty immune system in children, should be swept under the carpet, according to a new study by researchers at UCL and the London School of Hygiene and Tropical Medicine. .
In medicine, the "hygiene hypothesis" states that early childhood exposure to certain microorganisms protects against allergic diseases by contributing to the development of the immune system.
However, there is a widespread view (public narrative) that 21st century Western society is overly hygienic, meaning that young children are likely to be less exposed to germs in the first years of life and therefore , become less resistant to allergies.
In this article, published in the Journal of Allergy and Clinical Immunology , the researchers point to four important reasons that they say refute this theory and conclude that we are not "too clean for our own good."
Senior author, Emeritus Professor of Medical Microbiology Graham Rook (UCL Infection and Immunity), said:
"Exposure to microorganisms in early life is essential for the ’education’ of the immune and metabolic systems.
"The organisms that populate our intestine, skin and respiratory tract also play an important role in maintaining our health into old age: so throughout life we need to be exposed to these beneficial microorganisms, derived mainly from our mothers, other members of the family and the natural environment. .
"But for more than 20 years there has been a public narrative that hand and household hygiene practices, which are essential for stopping exposure to disease-causing pathogens, are also blocking exposure to beneficial organisms.
"In this paper, we set out to reconcile the apparent conflict between the need for cleanliness and hygiene to remain pathogen-free and the need for microbial input to populate our guts and shape our immune and metabolic systems."
In a review of the evidence, the researchers point to four factors.
- Firstly, the microorganisms found in a modern home are, to a significant degree, not those we need for immunity.
- Secondly, vaccines, in addition to protecting us from the infection they target, do much more to strengthen our immune system, so we now know that we do not have to risk dying by being exposed to pathogens.
- Third, we now have concrete evidence that microorganisms in the natural green environment are particularly important for our health; Domestic cleaning and hygiene do not influence our exposure to the natural environment.
- Finally, recent research shows that when epidemiologists find an association between household cleaning and health problems such as allergies, this is often not due to the elimination of organisms, but rather due to exposure of the lungs to cleaning products that They cause a type of disease. damage that favors the development of allergic responses.
Professor Rook added: "So household cleaning is good and personal cleaning is good , but, as explained in some detail in the paper, to prevent the spread of infection, you need to target the hands and surfaces involved with increased frequency in the transmission of infections. As we focus our cleaning practices, we also limit children’s direct exposure to cleaning agents.
"Exposure to our mothers, family members, the natural environment and vaccines can provide all the microbial inputs we need. These exposures do not conflict with selective hygiene or cleaning."
Conclusions We conclude that if we are guided by historical and evolutionary knowledge, we can identify the microbial exposures that are most essential to human physiology. We also conclude that this understanding, in the context of 21st century reality, is further enhanced when the recently revealed nonspecific benefits of vaccines and the likely TH2 adjuvantage of clearance agents are taken into consideration. Using this knowledge, we can be guided by modern microbiological risk assessments that identify critical moments and can reconcile these physiological needs for microbial exposure with appropriate hygiene practices (which may involve not only targeted cleaning of hands and surfaces, but also social distancing). social and the use of masks). to prevent airborne transmission) that minimize infection risks and minimize unnecessary exposure to cleaning agents. We are fully aware that there is an element of speculation in these conclusions. We cannot be sure that vaccines completely replace the nonspecific immune system, which stimulates the effects of infections, and we do not know the relative importance of the TH2 adjuvant effects of clearance agents. However, we hope we have provided a framework for a more nuanced discussion of how we can reconcile hygiene with a healthy immune system. |
















