Key points Is the addition of a long-acting muscarinic antagonist (LAMA) to inhaled corticosteroids (ICS) and long-acting β2-agonists (LABA) associated with differences in clinical outcomes and adverse events among people with moderate-to-moderate persistent asthma? to serious? Findings In this systematic review and meta-analysis that included 20 randomized clinical trials and 11,894 patients, triple therapy (ICS, LABA, and LAMA), compared with dual therapy (ICS plus LABA), was significantly associated with fewer severe asthma exacerbations (risk ratio, 0.83) and slightly better asthma control, but no significant differences in quality of life or most adverse events. Meaning Among patients with moderate to severe asthma, triple therapy compared with dual therapy was significantly associated with fewer severe asthma exacerbations and modest improvements in asthma control, but no significant differences in quality of life. |
Importance
The benefits and harms of adding long-acting muscarinic antagonists (LAMAs) to inhaled corticosteroids (ICS) and long-acting β2-agonists (LABAs) for moderate to severe asthma remain unclear.
Aim
To systematically synthesize outcomes and adverse events associated with triple therapy (ICS, LABA, and LAMA) versus dual therapy (ICS plus LABA) in children and adults with uncontrolled persistent asthma.
Data sources
MEDLINE, Embase, CENTRAL, ICTRP, FDA and EMA databases from November 2017 to December 8, 2020, without language restriction.
Study selection
Two investigators independently selected randomized clinical trials (RCTs) comparing triple versus dual therapy in patients with moderate to severe asthma.
Data extraction and synthesis
Two reviewers independently extracted data and assessed risk of bias. Random-effects meta-analyses were used, including exacerbation data at the individual patient level. The GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach was used to assess the certainty (quality) of the evidence.
Main results and measures
Severe exacerbations, asthma control (measured by the Asthma Control Questionnaire [ACQ-7], a 7-item list with each item ranging from 0 [completely controlled] to 6 [severely uncontrolled]; least important difference, 0, 5), quality of life (measured with the Asthma-Related Quality of Life [AQLQ] tool; score range, 1 [severe impairment] to 7 [no impairment]; least important difference, 0.5), mortality, and events adverse.
Results
Twenty RCTs using 3 types of LAMAs enrolling 11,894 children and adults (mean age, 52 years [range, 9-71 years]; 57.7% women) were included.
High-certainty evidence showed that triple therapy versus dual therapy was significantly associated with a reduced risk of severe exacerbations (9 trials [9932 patients]; 22.7% vs 27.4%; risk ratio, 0. 83 [95% CI, 0.77 to 0.90]) and an improvement in asthma control (14 trials [11,230 patients]; standardized mean difference [SMD], −0.06 [95% CI, −0.10 to −0.02]; mean difference on the ACQ-7 scale, −0.04 [95% CI, -0.07 to −0.01]).
There was no significant difference in asthma-related quality of life (7 trials [5247 patients]; SMD, 0.05 [95% CI, −0.03 to 0.13]; mean difference in AQLQ score, 0 .05 [95% CI, −0.03 to 0.13]; moderate-certainty evidence) or mortality (17 trials [11,595 patients]; 0.12% vs 0.12%; risk ratio, 0. 96 [95% CI, 0.33 to 2.75]; high-certainty evidence) between dual and triple therapy.
Triple therapy was significantly associated with an increase in dry mouth and dysphonia (10 trials [7395 patients]; 3.0% vs 1.8%; risk ratio, 1.65 [95% CI, 1.14 to 2.38]; high-certainty evidence), but treatment-related and serious adverse events were not significantly different between groups (moderate-certainty evidence).
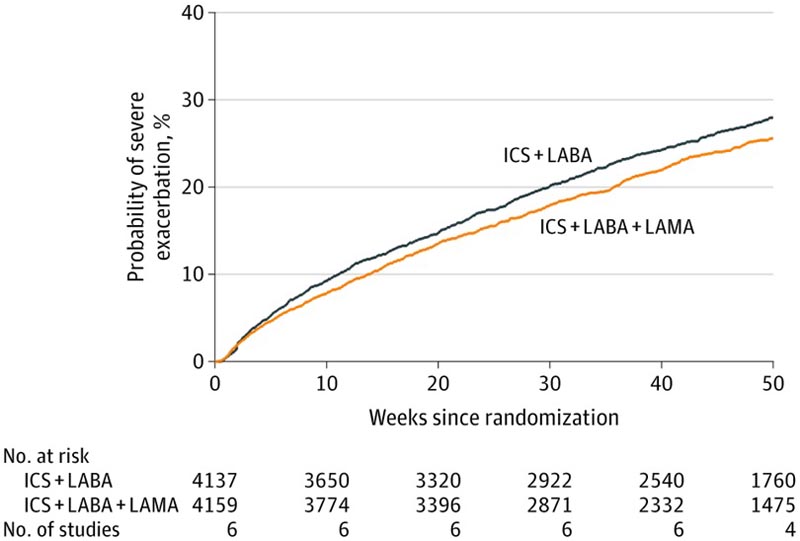
Severe asthma exacerbation was defined by the need for systemic steroids for ≥3 days, hospitalization, intensive care admission or intubation, or emergency department visits. Triple therapy indicates inhaled corticosteroids (ICS), long-acting β2-agonists (LABA), and long-acting muscarinic antagonists (LAMA), and dual therapy indicates ICS with a LABA. The hazard ratio (0.84 [95% CI, 0.77-0.92]) was calculated from the Cox regression model with shared frailty by study. Summary statistics per patient on observation time: mean (SD), 37.8 (16.5) weeks; median, 46.4 weeks (range, 0.2-52 weeks [interquartile range [IQR], 35.3-52.0 weeks, calculated under the assumption that IQR = 1.35 × SD).
Conclusions and relevance Among children (6 to 18 years) and adults with moderate to severe asthma, triple therapy, compared with dual therapy, was significantly associated with fewer severe asthma exacerbations and modest improvements in asthma control with no significant differences in quality of life or mortality. |
Discussion
In this systematic review and meta-analysis of 20 RCTs including 11,894 children (aged 6 to 18 years) and adults with uncontrolled moderate to severe asthma, triple therapy compared with dual therapy was significantly associated with fewer severe exacerbations and modest improvements in asthma control without significant differences in quality of life or mortality. No significant differences were observed in serious or treatment-related adverse events.
These findings are consistent with multiple lines of evidence supporting antimuscarinic protective effects against exacerbations. In preclinical and clinical studies, short-acting antimuscarinics improved airway bronchodilation and were associated with a lower risk of hospitalization during acute asthma and LAMAs protected against bronchoprovocation.
This is also consistent with study results demonstrating no subgroup differences in 3 types of LAMA in association with exacerbations supporting a class effect. In clinical practice, LAMAs may have additional benefits beyond reducing exacerbations.
The complementary bronchodilation properties of a LAMA to a LABA allow its use in patients who have developed tachyphylaxis to LABAs or in patients limited by the adverse effects of LABAs, such as tachycardia. Compared to biological therapies, LAMAs may be favorable in terms of independence of inflammatory phenotype, cost 10 and other contextual factors.
In this systematic review and meta-analysis, triple therapy was associated with statistically significant but potentially clinically unimportant benefits in asthma symptoms, and there were no significant differences between triple therapy and dual therapy with respect to related quality of life. with asthma. The changes in FEV1 were also small, but the clinical significance of these changes is difficult to qualify without minimum important difference thresholds established in patients with moderate to severe disease and receiving treatment with more than one class of bronchodilator.
The dissociation between asthma control indices and exacerbations is consistent with findings from previous studies in severe asthma. For example, several trials of biologic therapies have found a clinically important reduction in severe exacerbations with improvements in asthma symptoms below the minimal important difference. These findings may reflect a different pathophysiology between exacerbations and symptom control.
More generally, the results of this meta-analysis in asthma are similar to those in chronic obstructive pulmonary disease, showing a comparable direction and magnitude of association in exacerbations, quality of life, FEV1, and adverse events with triple therapy (CSI, LABA and LAMA) versus dual therapy (CSI plus LABA).















