Goals
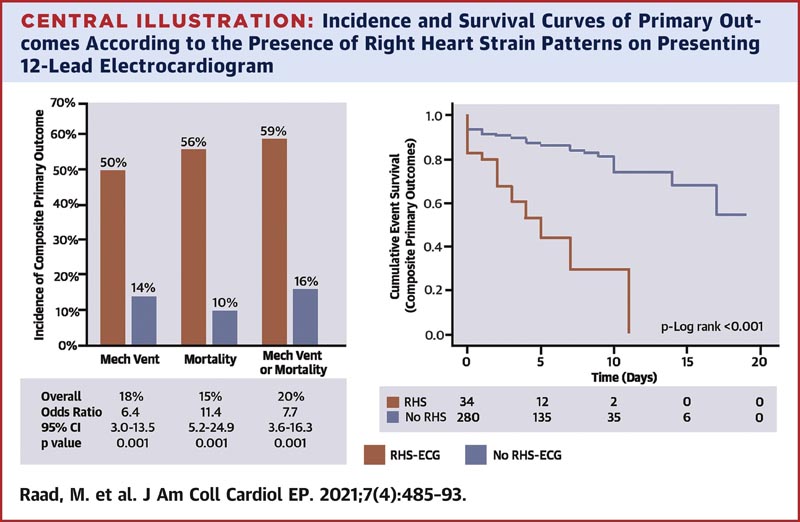
This study aimed to evaluate the association of new right heart stress patterns upon presentation of a 12-lead electrocardiogram (ECG-RHS) with outcomes in patients hospitalized with COVID-19.
Background
Cardiovascular comorbidities and complications, including right ventricular dysfunction, are common and associated with worse outcomes in patients with COVID-19. Data on the clinical utility of the 12-lead ECG to assist with prognosis are limited.
Methods
This study retrospectively evaluated the records of 480 patients who were consecutively admitted with COVID-19. ECGs obtained at presentation to the emergency department (ED) were considered index ECGs.
ECG-RHS (RV hypertrophy and/or overload) was defined by any new right axis deviation, S1Q3T3 pattern or ST depressions with T wave inversions in leads V1 to V3 or leads II, III and aVF.
Multivariable logistic regression was performed to assess whether ECG-RHS were independently associated with the primary outcomes.
Results
ED ECGs were available for 314 patients who were included in the analysis.
Most patients were in sinus rhythm, with sinus tachycardia being the most common dysrhythmia.
ECG-RHS findings were present in 40 (11%) patients.
ECG-RHS were significantly associated with the incidence of adverse outcomes and an independent predictor of mortality (adjusted odds ratio [adjOR]: 15.2; 95% confidence interval [CI]: 5.1 to 45.2; p <0.001), the need for mechanical ventilation (adjustment: 8.8, 95% CI: 3.4 to 23.2, p < 0.001) and their combination (adjustment: 12.1, 95% CI: 4, 3 to 33.9]; p <0.001).
Conclusions
|
Reference: Right Heart Strain on Presenting 12-Lead Electrocardiogram Predicts Critical. Mohamad Raad, Sarah Gorgis, Mohammed Dabbagh, Omar Chehab, Sachin Parikh, et al. J Am Coll Cardiol EP. 2021 Apr, 7 (4) 485–493