Recently, nephronophthisis (NPH) has been considered a monogenic cause of end-stage renal disease (ESRD) in adults. However, adult-onset NPH is difficult to diagnose accurately and has not been reported in a cohort study. In this study, we evaluated the genetic background and clinicopathological characteristics of NPH in adults. Methods We investigated 18 sporadic adult patients suspected of having PHN by renal biopsy. We analyzed 69 genes that cause hereditary cystic kidney disease and compared the clinicopathological findings between patients with and without pathogenic mutations in PHN-causing genes. Results Seven of 18 patients had NPH-causing pathogenic mutations in NPHP1, NPHP3, NPHP4, or CEP164. Compared with patients without pathogenic mutations, those with pathogenic mutations were significantly younger, but did not differ significantly in the classic pathological findings of NPH, such as tubular cysts. On the other hand, the number of tubules with duplication of the thick tubular basement membrane (TBM), which was defined as >10 μm thick, was significantly higher in patients with genetically proven adult NPH than in those without pathogenic mutations. α-smooth muscle actin (α-SMA)-positive myofibroblasts were detected within the thick TBM duplication. Conclusions In adult patients with NPH, thick TBM duplication was the specific finding. Our analysis also suggested that older patients tended not to have pathogenic mutations, even when they were suspected of having PHN by renal biopsy. These findings could be the new clinical clue for the diagnosis of NPH in adult patients. Discussion To the best of our knowledge, this was the first cohort study to investigate the clinicopathological findings and genetic background of adult patients with NPH. Through genetic analysis of 18 adult patients with suspected NPH by renal biopsy, we found pathogenic mutations related to NPH in 7 patients. Compared with patients who did not have pathogenic mutations, adult patients who had genetically proven NPH were significantly younger and had a significantly higher proportion of males, a significantly lower incidence of hypertension, and a significantly higher number of tubules with thickened TBM duplication. . |
Pathological findings specific to adult-onset NPH
The 3 pathologic findings known to be specific for NPH were not significantly different between adult patients with NPH and those who did not have a mutation causing NPH. Therefore, we looked for more novel pathological findings that were specific to adult PNH cases.
We focused on TBM duplication, which was reported as another specific finding in NPH. Although TBM duplication has been reported in non-hereditary kidney diseases, we noted that TBMs were quite thick and reduplicated in genetically proven adult NPH cases.
Therefore, we focused on the thickness of the TBM duplication; we defined thick TBM duplication as >10 μm. Interestingly, the number of tubules with thick TBM duplication was significantly higher in genetically tested adult NPH than in those without pathogenic mutation.
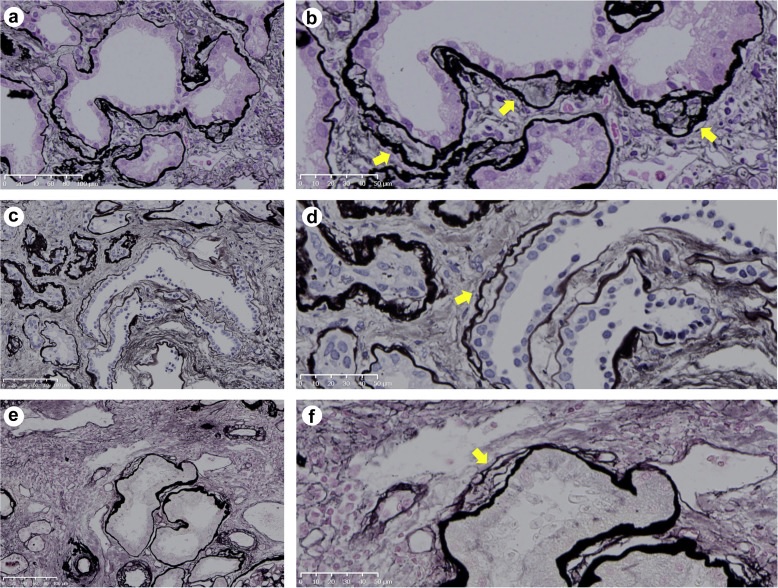
Duplication of thick tubular basement membrane. Duplication of the thick tubular basement membrane was defined as a thickness of >10 μm (yellow arrows). (a and b) Patient number 883, periodic acid-methenamine silver (PAM) stain, 20× and 40× magnification, respectively. (c and d) Patient number 478, PAM staining, 20× and 40× magnification, respectively. (e and f) Patient number 896, PAM staining, 20× and 40× magnification, respectively. All slides were scanned on the NanoZoomer NDP system with a resolution of 40 × (0.23 μm/pixel) (Hama-matsu Photonics, Hamamatsu-City, Japan).
Comments
What is nephronophthisis? Under the concept of nephronophthisis (NPHP), also formerly known as nephronophthisis-medullary cystic disease complex (NPHP-MCKD) and currently as ciliopathies related to nephronophthisis (NPHP-RC), we find a group of diseases that present histological, clinical and common pathophysiological conditions that are a consequence of mutations in multiple genes that encode proteins involved in the composition and correct functioning of the ciliary apparatus (basal bodies, primary cilia and centrosomes). These mutations, classically monogenic and of autosomal recessive inheritance, will lead to the development of renal cystic diseases associated or not with manifestations in other organs and with a progression typically towards end-stage chronic kidney disease (ESRD) in the first two decades of life. Due to the clinical and genetic differences and the prognostic implications associated with the age of onset of the disease, a classification has been carried out based on the average age at which ESRD develops, thus dividing it into three types.
Each of them associates specific genetic defects and has as a common factor the development of chronic tubulointerstitial nephritis with alterations in the ability to concentrate urine, together with sodium reabsorption deficiency in some cases, and in all of them typically maintaining a sediment at the beginning. urinary tract without alterations (mild initial low molecular weight proteinuria in some patients). |
Researchers from Tokyo Medical and Dental University (TMDU) in a pioneering study identify clinical, genetic and histopathological features that can help confirm the diagnosis when nephronophthisis occurs in adults
Nephronophthisis (NPH) is a kidney disease that mainly affects children. Now, for the first time, researchers at Tokyo Medical and Dental University (TMDU) have studied several adults with NPH and highlighted clinical, genetic and pathological features that could help confirm this challenging diagnosis.
NPH is inherited in an autosomal recessive pattern and, although rare, is the most common genetic cause of kidney failure in children. The name is derived from ’nephron’ , the functional filtration units of the kidney, and ’phthisis’ , which is Greek for ’wasting’.
Recent genetic studies have highlighted that NPH can also occur in adults , resulting in end-stage renal disease (ESRD). However, there are only a few case reports and no cohort studies, possibly due to rarity and diagnostic difficulties.
The clinical diagnosis of NPH in adults is problematic because the clinical, radiological, and histological features are non-specific.
Even extrarenal features are less in adults. Since treatment includes kidney transplant and genetic counseling, accurate early diagnosis is essential. Takuya Fujimaru, first author, explains more.
"Currently, molecular genetic analysis is the only practical method to clinically diagnose NPH. However, as more than 25 genes have been identified, Sanger sequencing (one DNA fragment at a time) is tedious; complete mutations using next generation sequencing (NGS). Therefore, the ability to sequence millions of fragments is required. Unfortunately, NGS is expensive and has limited availability. Therefore, we aimed to investigate the genetic background of adult nephronophthisis and evaluate the clinical characteristics and pathological changes in these patients."
The research team, drawn from leading medical institutions in Japan, studied 18 patients with adult-onset NPH suspected from a kidney biopsy using cutting-edge tools such as low-vacuum scanning electron microscopy and capture-based sequencing.
They analyzed 69 genes associated with kidney disease and compared patients with and without mutations. Seven of their patients had NPH-causing mutations; They were comparatively young, although not significantly different in classic pathological findings. Interestingly, however, duplication of thickened tubular basement membrane (TBM) was observed in many more tubules in these genetically tested patients.
"Our finding that thickened tubular basement membrane (TBM) duplication is specific to adult-onset NPH is significant," says corresponding author Eisei Sohara. "The number of tubules showing this pathological change has potential as a diagnostic criterion for NPH in adults. We also observed that older patients are unlikely to have pathogenic mutations; this could be a novel diagnostic indicator, through comprehensive testing against a target panel of associated genes remains necessary.















