The American College of Gastroenterology published updated guidelines for the treatment of patients with lower gastrointestinal bleeding (LBGI).
Background
Acute lower gastrointestinal bleeding (LBGI) causes more than 100,000 admissions in the US annually and the incidence appears to be increasing based on current literature.
There are a significant number of etiologies for acute lower gastrointestinal bleeding (LBGI). Diverticulosis is the most common cause, although it varies depending on the population. Other causes include ischemic colitis, hemorrhoids, angioectasias, colorectal neoplasia, postpolypectomy hemorrhage, colitis (inflammatory, infectious, or radiation-related), rectal/stercoral/NSAID-induced ulcers, and radiation proctopathy.
Important risk factors for acute lower gastrointestinal bleeding (LBGI) include the use of antiplatelet agents such as aspirin, NSAIDs, and P2Y12 inhibitors such as clopidogrel, older age, and diverticulosis.
| Recommendation Rating and Strength |
• Strong recommendation – Evidence shows that the benefit of the intervention or treatment clearly outweighs any risks. • Conditional recommendation : there is uncertainty about the risk/benefit ratio. • High certainty of the evidence : further research is unlikely to change confidence in the effect estimate. • Moderate certainty of evidence – further research is likely to have a significant impact and may change the estimate. • Low certainty of evidence : further research is very likely to change the estimate. |
| Triage/initial evaluation |
> Key concept : A specific history, physical examination, and laboratory evaluation should be obtained at the time of patient presentation to evaluate the severity of the bleeding and its possible location and etiology.
Initial patient evaluation and hemodynamic resuscitation should be performed simultaneously.
| Risk assessment |
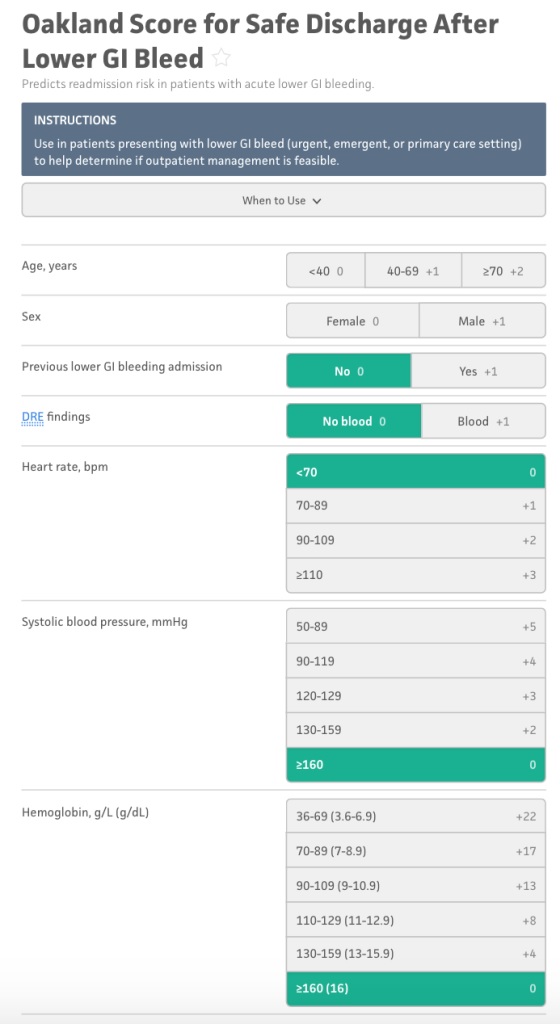
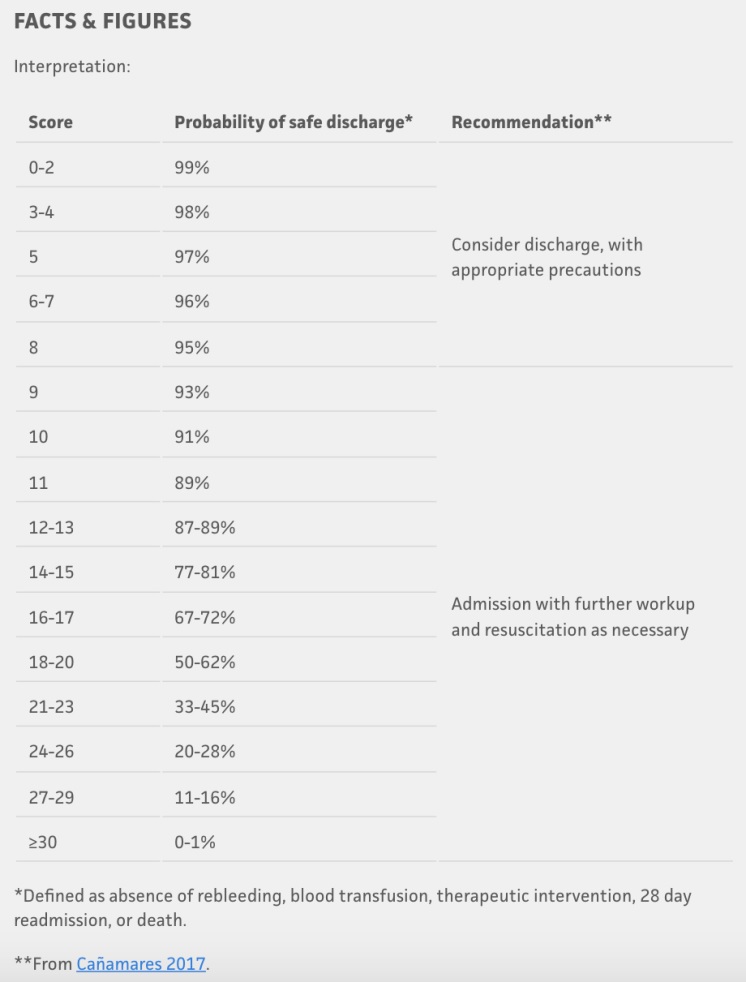
> Recommendation : We suggest using risk stratification tools (e.g., Oakland score #8) to identify low-risk patients with LGIB who are appropriate for early discharge and outpatient diagnostic evaluation. Risk scores should be used to complement, but not replace , medical judgment. (Conditional recommendation, low quality evidence).
| Hemodynamic resuscitation |
> Key concept : Patients with hemodynamic instability and/or suspected ongoing hemorrhage should receive intravenous fluid resuscitation with the goal of optimizing blood pressure and heart rate before endoscopic evaluation/intervention.
> Recommendation: We suggest a restrictive red blood cell transfusion strategy(transfusion threshold at a hemoglobin level of 7 g/dL) in hemodynamically stable patients with LGIB. (Conditional recommendation, low quality evidence).
| Exclusion of proximal source of bleeding. |
> Key concept : Hematochezia associated with hemodynamic instability may be indicative of a source of UGIB and upper endoscopy should be performed if suspicion is high to exclude a proximal source of bleeding.
| Management of patients with antivitamin K (VKA) |
> Key concept : Endoscopic hemostasis can be considered safe and effective in patients who have an international normalized ratio (INR) of 2.5 or less.
> Recommendation : Although most patients with LGIB treated with VKA are unlikely to require reversal, we suggest reversal for patients who present with life-threatening LGIB and have an INR that substantially exceeds the therapeutic range.
For patients receiving vitamin K antagonists (VKAs) to prevent stroke in non-valvular atrial fibrillation requiring reversal, 4-factor prothrombin complex concentrate (PCC) is preferred over fresh frozen plasma (FFP) due to the rapidity of INR reduction (conditional recommendation, very low quality evidence). .
| Reversal of oral anticoagulation with direct oral anticoagulants (DOACs) |
> Recommendation : For patients taking direct-acting oral anticoagulants (DOACs), we suggest reversal for the small subset of patients who present with life-threatening acute lower gastrointestinal bleeding (LBGI) that does not respond to initial resuscitation and cessation of the anticoagulant only.
For patients requiring reversal , targeted reversal agents (idarucizumab for dabigatran and andexanet alfa for apixaban and rivaroxaban) should be used when available if the DOAC was taken within the last 24 hours (conditional recommendation, very low quality evidence) .
| Management of antiplatelets in an acute setting |
> Key concept : Platelets should be administered in the setting of severe acute lower gastrointestinal bleeding (LBGI) to maintain a platelet count of >30 × 109/L, and a higher threshold of >50 × 109/L may be considered. if endoscopic procedures are required.
Routine platelet transfusion provides no benefit to patients taking antiplatelet agents.
> Key concept: For patients with acute lower gastrointestinal bleeding (LBGI) taking aspirin for secondary cardiac prevention, aspirin should beduring hospitalization if possible. Non-aspirin antiplatelet agents should initially bein patients with severe hematochezia. However, for patients with recent cardiac stents within 1 year, a multidisciplinary approach should be used to determine the safety of temporarily discontinuing antiplatelets.
| Role of antifibrinolytic agents |
> Recommendation : We do not recommend the administration of antifibrinolytic agents such as tranexamic acid in acute lower gastrointestinal bleeding (LBGI). (Strong recommendation, moderate quality evidence).
| Role of colonoscopy |
> Key concept : The colonic mucosa should be carefully inspected during insertion and removal, with aggressive attempts to wash away residual feces and blood to identify bleeding sites. The terminal ileum should be intubated to exclude proximal bleeding sources when possible if a colonic bleeding source is not found. The use of a transparent cap is recommended to aid in the detection and treatment of bleeding.
> Recommendation : We recommend colonoscopy for most patients who are hospitalized with lower gastrointestinal bleeding (LGIB) due to its value in detecting a source of bleeding (strong recommendation, low quality evidence).
> Recommendation: However, colonoscopy may not be necessary in patients where bleeding has decreased and the patient has had a high-quality colonoscopy within 12 months with adequate bowel preparation showing diverticulosis without colorectal neoplasia. (Conditional recommendation, very low quality evidence).
| Role of call to action |
> Recommendation: We suggest performing CT angiography as an initial diagnostic test in patients with ongoing hemodynamically significant hematochezia. However, CTA has poor performance in patients with minor LGIB or in those in whom bleeding has clinically decreased. (Conditional recommendation, low quality evidence).
| Management of positive CT angiography |
> Recommendation: We recommend that patients who have a CTA that demonstrates extravasation be immediately referred to interventional radiology for transcatheter arteriography and possible embolization . In specialized centers with experience in performing endoscopic hemostasis, colonoscopy may also be considered after a positive CTA. (Strong recommendation, moderate quality evidence).
| Timing of the colonoscopy |
> Recommendation : For hospitalized patients with LGIB who require colonoscopy, we recommend performing non-emergency in-hospital colonoscopy becauseperforming urgent colonoscopy within 24 hours has not been shown to improve clinical outcomes, such as rebleeding and mortality . (Strong recommendation, moderate quality evidence).
| Role of treatment of stigmata of recent hemorrhage. |
> Key concept : Endoscopic therapy is recommended when active bleeding or stigmata of recent hemorrhage (RHR) is found, regardless of etiology.
| Treatment of diverticular hemorrhage |
> Recommendation : When detected, we recommend treatment of diverticular stigma (SRH) with clips through the endoscope, endoscopic band ligation (EBL) or coagulation. (Strong recommendation, moderate quality evidence).
| Role of repeat colonoscopy, angiography and surgery |
> Key concept : For patients who experience new bleeding after initial hemostasis or cessation of bleeding, repeat colonoscopy may be considered depending on the stability of the patient and the likelihood of successfully repeating endoscopic therapy. In patients with suspected recurrent diverticular hemorrhage with recent colonoscopy who are hemodynamically stable, observation may be considered.
| Resumption of antiplatelet medications and risk of recurrence |
> Recommendation : We recommend discontinuing non-aspirin NSAIDs after hospitalization for diverticular hemorrhage. (Strong recommendation, low quality evidence).
> Recommendation: We suggest discontinuing aspirin for primary cardiovascular preventionafter hospitalization for diverticular hemorrhage given the risk of recurrent diverticular hemorrhage. (Conditional recommendation, low quality evidence).
> Recommendation: We suggest continuing aspirin after hospitalization for diverticular hemorrhage in patients with an established history of cardiovascular disease, given the benefits of reducing future ischemic events. (Conditional recommendation, low quality evidence).
> Recommendation: We recommend that providers reevaluate the risks versus benefits of continuing non-aspirin antiplatelet agents , such as P2Y12 receptor antagonists, in a multidisciplinary setting after hospitalization for diverticular hemorrhage, given the demonstrated risks of recurrent diverticular hemorrhage. (Strong recommendation, low quality evidence).
| Resumption of anticoagulants and risk of recurrence. |
> Recommendation: We recommend resuming anticoagulation after cessation of lower gastrointestinal bleeding (LBGI), as resuming anticoagulation has been shown to decrease the risks of postbleeding thromboembolism and mortality. (Strong recommendation, moderate quality evidence).
| Final summary and strength of recommendations |
1. We suggest using risk stratification tools (e.g., Oakland Score #8) to identify low-risk patients with LGIB who are appropriate for early discharge and outpatient diagnostic evaluation. Risk scores should be used to complement, but not replace, medical judgment. (Conditional recommendation, low quality evidence) 2. We suggest a restrictive RBC transfusion strategy (transfusion threshold at a hemoglobin level of 7 g/dL) in hemodynamically stable patients with LGIB. (Conditional recommendation, low quality evidence) 3. Although most patients with LGIB taking vitamin K antagonists are unlikely to require reversal, we suggest reversal for patients who present with life-threatening LGIB and have an INR that substantially exceeds the range. therapeutic. For patients taking vitamin K antagonists to prevent stroke in patients with non-valvular atrial fibrillation requiring reversal, 4-factor PCC is preferred over FFP due to the rapidity of INR reduction. (Conditional recommendation and very low quality evidence) 4. For patients taking direct oral anticoagulants, we suggest reversal for the small subset of patients who present with life-threatening LGIB unresponsive to initial resuscitation and discontinuation of anticoagulant alone. For patients requiring reversal, targeted reversal agents (idarucizumab for dabigatran and andexanet alfa for apixaban and rivaroxaban) should be used when available if direct oral anticoagulant has been taken within the last 24 hours. (Conditional recommendation, very low quality evidence) 5. We do not recommend the administration of antifibrinolytic agents such as tranexamic acid in LGIB. (Strong recommendation, moderate quality evidence) 6a. We recommend colonoscopy for most hospitalized patients with LGIB because of its value in detecting a source of bleeding. (Strong recommendation, low quality evidence) 6b. However, colonoscopy may not be necessary in patients in whom bleeding has decreased and the patient has had a high-quality colonoscopy within 12 months with adequate bowel preparation showing diverticulosis without colorectal neoplasia. (Conditional recommendation, very low quality evidence) 7. We suggest performing CT angiography as an initial diagnostic test in patients with ongoing hemodynamically significant hematochezia. However, CT angiography is of poor performance in patients with minor LGIB or in those in whom bleeding has clinically decreased. (Conditional recommendation, low quality evidence) 8. We recommend that patients who undergo CT angiography that demonstrates extravasation be immediately referred to interventional radiology for transcatheter treatment and possible embolization. For specialized centers with experience performing endoscopic hemostasis, colonoscopy may also be considered after positive CT angiography. (Strong recommendation, moderate quality evidence) 9. For hospitalized patients with LGIB who require a colonoscopy, we recommend performing a non-emergency in-hospital colonoscopy, as performing an urgent colonoscopy within 24 hours has not been shown to improve clinical outcomes, such as the new hemorrhages and mortality. (Strong recommendation, moderate quality evidence) 10. When detected, we recommend treating diverticular stigmata of hemorrhage with clips through the endoscope, endoscopic band ligation, or coagulation. (Strong recommendation, moderate quality evidence) 11a. We recommend discontinuing non-aspirin NSAIDs after hospitalization for diverticular bleeding. (Strong recommendation, low quality evidence). 11b. We suggest discontinuing aspirin for primary cardiovascular prevention after hospitalization for diverticular hemorrhage given the risks of recurrence of diverticular hemorrhage. (Conditional recommendation, low quality evidence) 11c. We suggest continuing aspirin after hospitalization for diverticular hemorrhage in patients with an established history of cardiovascular disease given the benefits of reducing future ischemic events. (Conditional recommendation, low quality evidence) 11d. We recommend that providers reevaluate the risks versus benefits of continuing non-aspirin antiplatelets, such as P2Y12 receptor antagonists, in a multidisciplinary study after hospitalization for diverticular hemorrhage given the demonstrated risk of recurrent diverticular hemorrhage. (Strong recommendation, low quality evidence) 12. We recommend resuming anticoagulation after discontinuing LGIB since resuming anticoagulation has been shown to decrease the risks of postbleeding rhomboembolism and mortality. (Strong recommendation, moderate quality evidence). |
| Abbreviations : CT, computed tomography; FFP, fresh frozen plasma; INR, international normalized ratio; LGIB, lower gastrointestinal bleeding; NSAID, non-steroidal anti-inflammatory; PCC, prothrombin complex concentrate; PRBC, concentrated red blood cells. |















