Benign prostatic hyperplasia (BPH) is a pathological diagnosis that is often used to refer to a collection of symptoms (often called lower urinary tract symptoms [LUTS]) in older men. LUTS typically include storage symptoms, such as urinary frequency and nocturia, and voiding symptoms, such as weak stream. While prostate enlargement due to BPH contributes significantly to LUTS, age-related changes in the bladder, metabolic syndrome, and vascular diseases also play a role.
Globally, approximately 1 in 4 men will have BPH-related lower urinary tract symptoms (LUTS) in their lifetime, and the prevalence increases with age.
There is a considerable risk of worsening LUTS over time, and men generally seek treatment only when their symptoms cause significant discomfort. Current treatment guidelines suggest initiating treatment based on the degree of bothersomeness of symptoms.
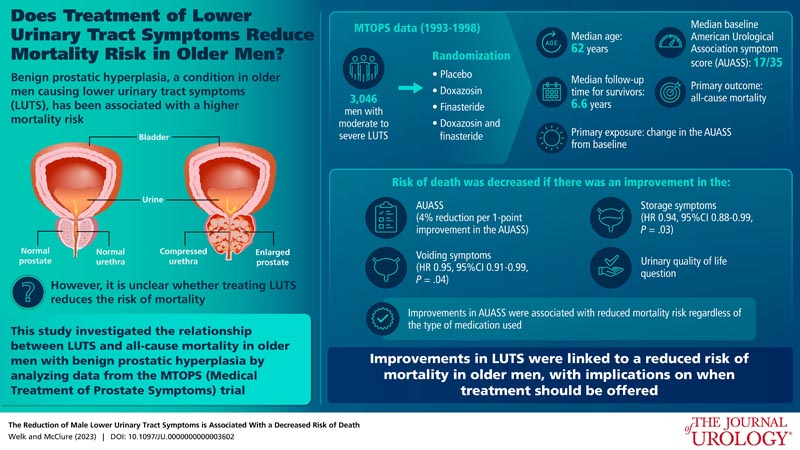
Studies have reported a significantly increased risk of mortality with worse LUTS; While most research has focused on nocturia, male LUTS in general may also be associated with an increased risk of death. However, this observed relationship may be due to the confounding effects of frailty or cardiovascular disease (which are associated with both mortality and LUTS). Additional studies examining the association between LUTS and mortality are needed. Our objective was to determine whether improvement in male LUTS in the context of medical treatment is associated with a reduced risk of mortality.
Graphic summary
Aim:
Male lower urinary tract symptoms have been correlated with an increased risk of death; However, it is not clear whether treatment will reduce this risk. Our objective was to determine whether a reduction in lower urinary tract symptoms is associated with a reduced risk of mortality.
Materials and methods:
We performed a secondary analysis of the MTOPS (Medical Treatment of Prostate Symptoms) randomized trial of placebo, doxazosin, finasteride, or doxazosin and finasteride. Men in the United States between 1993 and 1998 who were > 50 years of age with moderate to severe lower urinary tract symptoms were included.
We used several Cox regression models to evaluate the relationship between AUA symptom score (modeled as a time-varying exposure) and death.
Results:
A total of 3046 men (mean age 62, quartiles 57-68) were randomized and had a baseline AUA symptom score. For every 1-point improvement in the AUA symptom score, the hazard ratio for death was 0.96 (0.94-0.99, p = 0.01).
Our sensitivity analyzes found a similar significant reduction in the hazard ratio of death among men who received active treatment, but not among men who were randomly assigned to the placebo group; Our results did not change when men were censored at the time of transurethral resection of the prostate, with adjustment for potential confounders, or with a shorter observation period after the last study visit.
A comparable significant reduction in mortality was seen with 1-point improvements in storage (HR 0.94, 95% CI 0.88-0.99, P = 0.04) and voiding subscales (HR 0.94, 95% CI 0.88-0.99, P = 0.04). 95, 95% CI: 0.91-0.99, P = 0.03) individually.
Conclusions: An improvement in the AUASS of older men with BPH is associated with a decreased risk of mortality over 6 years. Improvements in storage and urination symptoms are significantly associated with a lower risk of death. More studies are needed to see whether early treatment of LUTS independently decreases the risk of mortality. |
Discussion
We used data from existing, well-known randomized trials of MTOPS ( Medical Treatment of Prostate Symptoms ) to evaluate whether an improvement in urinary symptoms is independently associated with mortality risk among men with BPH. We found that there was a statistically significant decrease in mortality risk of 4% for every 1-point improvement on the AUASS. Although this is a small decrease, it is clinically quite significant given the importance of the result.
A similar and statistically significant decrease in mortality risk was observed when a 1-point improvement was observed in storage symptoms alone (6%) or micturition symptoms alone (5%).
The point estimate for the single nocturia question was in a similar direction (10% reduction in mortality for every 1-point improvement); however, it was not statistically significant, possibly as a result of decreased discriminatory power, as there was only one question measuring nocturia on the AUASS.
We did not show an effect in the placebo group, which may mean that active treatment is necessary to reduce the risk of mortality, or this may be a result of a lower rate of improvement on the AUASS in this group and reduced statistical power. ; It is also important to remember that this is a subgroup analysis and therefore should not be given too much importance.
Our results are unique as, to our knowledge, this is the first study to examine whether an improvement in male LUTS is associated with a lower risk of death, rather than showing an association between the degree of LUTS and mortality. Our results are consistent with the other studies in this area. A large Finnish longitudinal study found that among 3,143 men over the age of 50 who were surveyed repeatedly over 15 years, a greater magnitude of LUTS from storage or urination increased the risk of death by 10% to 20%. The individual symptoms of frequency, nocturia, and urge incontinence were most relevant to mortality risk. Nocturia specifically has been well studied in relation to mortality risk. A recent meta-analysis of 11 studies found that ≥2 episodes of nocturia were associated with a 27% increased risk of mortality (or a 1.6% absolute risk increase in people older than 60 years). Similarly, a secondary analysis of the REDUCE (Dutasteride Reduction of Prostate Cancer Events) trial showed that nocturia, defined as ≥3 voids per night, was associated with a 72% increased risk of death.
The relationship between urinary symptoms and mortality could be an association , whereby urinary symptoms are a marker of cardiovascular disease, obesity, sleep apnea, diabetes, or early neurological disease with urinary symptoms. However, this would seem to be less likely in the context of our study results, as it is not clear why improving LUTS through treatment would reduce mortality risk if these mortality risks are due to underlying disease. It is also possible that medications used to treat urinary symptoms may directly decrease mortality risk through non-urological effects .
For example, alpha-1 blockers may decrease the risk of mortality in adults with respiratory infections (perhaps by altering cytokine release), and finasteride may decrease the risk of bladder cancer. However, in this situation we would expect death to be significantly lower, and this was not the case in either the analysis based on randomization or in our adjusted models.
Finally, it could be a causal relationship, whereby urinary symptoms affect sleep, increase the risk of falls and fractures, and negatively affect quality of life and mental health. This would mean that successful treatment of these symptoms directly decreases the risk of death. The above causal mechanisms are plausible, given the causes of death we saw among MTOPS participants; For example, poor sleep is strongly correlated with cardiovascular disease, and minor depression is correlated with cardiovascular death in older men.
This study has direct implications for clinical practice . Currently, urinary symptoms are generally considered a benign condition and patients are treated if they have significant discomfort. However, symptomatic discomfort does not perfectly correlate with the degree of symptoms (the correlation between the AUASS total and the discomfort question is 0.7812); therefore, it is possible that if there is a causal association between LUTS and mortality, earlier intervention based solely on symptom level would be appropriate. This would be analogous to the primary care approach to systolic blood pressure control , where there is a linear increase in mortality risk with increasing systolic blood pressure starting even between 125 and 129 mm Hg, but is reduced with treatment. . Our research is especially timely given the wide range of conservative options, medications, and minimally invasive surgical options that are now available to treat male LUTS. Although the magnitude of the decrease in the risk of death was low, for an outcome like mortality this is very important.
Final message
- Improvement in male lower urinary tract symptoms was associated with a reduced risk of death.
- More studies are needed to determine whether the male treatment paradigm should shift toward treating symptoms regardless of complaints.















