COLUMBIA UNIVERSITY IRVING MEDICAL CENTER
Summary Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the pathogen responsible for the coronavirus disease 2019 (COVID-19) pandemic, which has led to global healthcare crises and overstretched healthcare resources. As the population of patients recovering from COVID-19 grows, it is critical to establish an understanding of the healthcare issues surrounding them. COVID-19 is now recognized as a multi-organ disease with a wide spectrum of manifestations. Similar to post-acute viral syndromes described in survivors of other virulent coronavirus epidemics, there are increasing reports of persistent and prolonged effects after acute COVID-19. Patient advocacy groups, many of whom identify themselves as long-haulers , have contributed to the recognition of post-acute COVID-19 , a syndrome characterized by persistent symptoms and/or late or long-term complications beyond the 4 weeks from the onset of the disease. Here, we provide a comprehensive review of the current literature on post-acute COVID-19, its pathophysiology, and its organ-specific sequelae. Finally, we discuss considerations relevant to the multidisciplinary care of COVID-19 survivors and propose a framework for the identification of those at high risk for post-acute COVID-19 and their coordinated management through dedicated COVID-19 clinics. |
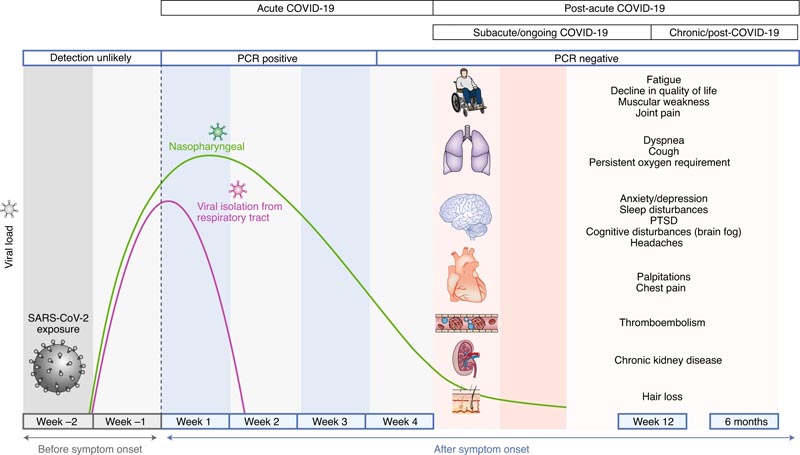
Acute COVID-19 usually lasts up to 4 weeks from the onset of symptoms, beyond which SARS-CoV-2 with the capacity to replicate has not been isolated. Post-acute COVID-19 is defined as persistent symptoms and/or late or long-term complications beyond 4 weeks from symptom onset. Common symptoms seen in post-acute COVID-19 are summarized.
Pathophysiology
The predominant pathophysiological mechanisms of acute COVID-19 include the following:
- Direct viral toxicity
- Endothelial damage and microvascular damage
- Deregulation of the immune system
- Stimulation of a hyperinflammatory state
- Hypercoagulability with resulting in situ thrombosis and macrothrombosis
- Maladaptation of angiotensin-converting enzyme pathway 2 (ACE2).
The overlap of the sequelae of post-acute COVID-19 with those of SARS and MERS may be explained by phylogenetic similarities between the responsible pathogenic coronaviruses. The overlap of SARS-CoV-2 genomic sequence identity is 79% with SARS-CoV-1 and 50% with MERS-CoV28,29. Furthermore, SARS-CoV-1 and SARS-CoV-2 share the same host cell receptor: ACE2.
However, there are notable differences, such as the higher affinity of SARS-CoV-2 for ACE2 compared to SARS-CoV-1, which is likely due to differences in the receptor-binding domain of the spike protein that mediates the contact with ACE2.
In contrast to the other structural genes, the spike gene has diverged in SARS-CoV-2, with only 73% amino acid similarity to SARS-CoV-1 in the receptor binding domain of the spike protein. the spike30. Furthermore, an additional S1-S2 cleavage site in SARS-CoV-2 allows for more efficient cleavage by host proteases and facilitates more efficient binding. These mechanisms have likely contributed to more efficient and widespread transmission of SARS-CoV-2.
Possible mechanisms contributing to the pathophysiology of post-acute COVID-19 include:
(1) Virus-specific pathophysiological changes.
(2) Immune aberrations and inflammatory damage in response to acute infection.
3) Expected consequences of a post-critical illness.
While the first two are discussed in more detail in the organ-specific sections below, post-intensive care syndrome is now well recognized and includes new or worsening abnormalities in physical, cognitive, and psychiatric domains following critical illness. The pathophysiology of post-intensive care syndrome is multifactorial and has been proposed to involve ischemia and microvascular injury, immobility, and metabolic alterations during critical illness.
Additionally, similar to previous studies of SARS survivors, 25-30% of whom experienced secondary infections, survivors of acute COVID-19 may be at increased risk of infections from bacteria, fungi (pulmonary aspergillosis), or other pathogens. . However, these secondary infections do not explain the persistent and prolonged sequelae of post-acute COVID-19.
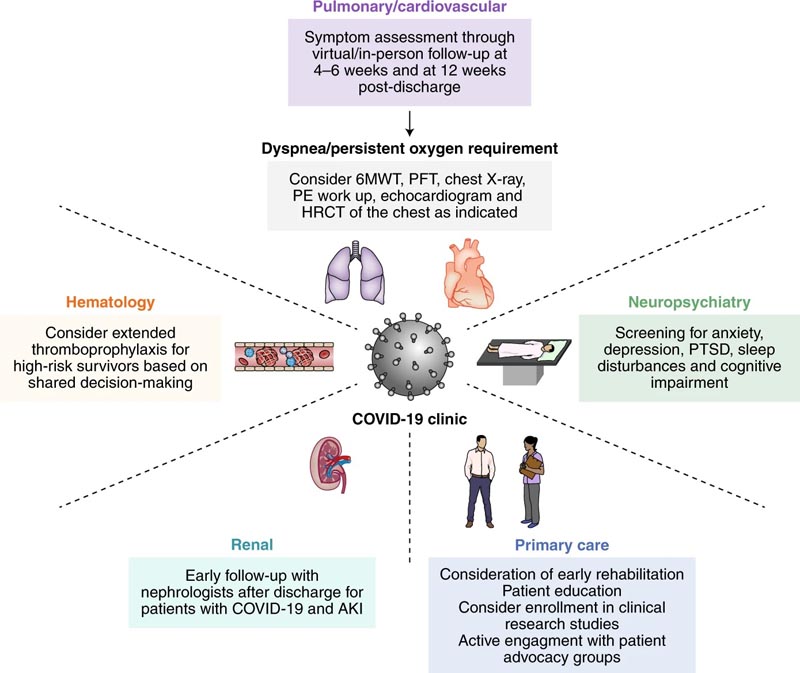
Multidisciplinary collaboration is essential to provide integrated outpatient care to acute COVID-19 survivors in COVID-19 clinics. Depending on resources, prioritization may be considered for those at high risk for post-acute COVID-19, defined as those with severe illness during acute COVID-19 and/or need for care in an ICU, advanced age, and presence of organic comorbidities. . (pre-existing respiratory disease, obesity, diabetes, hypertension, chronic cardiovascular disease, chronic kidney disease, post-organ transplant or active cancer). The pulmonary/cardiovascular management plan was adapted from a guidance document for patients hospitalized with COVID-1976 pneumonia. HRCT, high-resolution computed tomography; PE, pulmonary embolism.
Summary of Post-Acute COVID-19 by Organ System Dyspnea, decreased exercise capacity, and hypoxia are usually persistent symptoms and signs. Reduced diffusing capacity, restrictive lung physiology, and ground-glass opacities and fibrotic changes have been observed on imaging during follow-up of COVID-19 survivors. Evaluation of progression or recovery of lung disease and function may include home pulse oximetry, 6MWT, PFT, high-resolution chest CT, and CT pulmonary angiography as clinically appropriate. Hematological Thromboembolic events have been observed to be <5% in post-acute COVID-19 in retrospective studies. The duration of the hyperinflammatory state induced by SARS-CoV-2 infection is unknown. Direct oral anticoagulants and low molecular weight heparin may be considered for prolonged thromboprophylaxis after risk-benefit discussion in patients with predisposing risk factors for immobility, persistently elevated D-dimer levels (more than twice the upper limit than normal) and risk of comorbidities such as cancer Cardiovascular Persistent symptoms may include palpitations, dyspnea, and chest pain. Long-term sequelae may include increased cardiometabolic demand, myocardial fibrosis or scarring (detectable by cardiac MRI), arrhythmias, tachycardia, and autonomic dysfunction. Patients with cardiovascular complications during an acute infection or those who experience persistent cardiac symptoms can be monitored with serial clinical, echocardiographic, and electrocardiographic follow-up. Neuropsychiatric Persistent abnormalities may include fatigue, myalgia, headache, dysautonomia, and cognitive impairment (brain fog). Anxiety, depression, sleep disorders, and post-traumatic stress disorder have been reported in 30-40% of COVID-19 survivors, similar to survivors of other pathogenic coronaviruses. The pathophysiology of neuropsychiatric complications is mechanistically diverse and involves immune dysregulation, inflammation, microvascular thrombosis, iatrogenic effects of medications, and psychosocial impacts of infection. Renal Resolution of AKI during acute COVID-19 occurs in the majority of patients; however, a reduction in eGFR has been reported at 6 months of follow-up VANOC may be the predominant pattern of kidney injury in people of African descent COVID-19 survivors with persistent kidney failure may benefit from early and close follow-up at AKI survivor clinics Endocrine Endocrine sequelae may include new or worsening control of existing diabetes mellitus, subacute thyroiditis, and bone demineralization. Patients with newly diagnosed diabetes in the absence of traditional risk factors for type 2 diabetes, with suspected hypothalamic-pituitary-adrenal axis suppression or hyperthyroidism should undergo appropriate laboratory testing and be referred to endocrinology. Gastrointestinal and hepatobiliary Prolonged viral fecal shedding may occur in COVID-19 even after a negative nasopharyngeal swab test COVID-19 has the potential to alter the gut microbiome, including enrichment of opportunistic organisms and depletion of beneficial commensals. Dermatological Hair loss is the predominant symptom and has been reported in approximately 20% of COVID-19 survivors. Criteria Diagnostic criteria: <21 years with fever, elevated inflammatory markers, multiple organ dysfunction, current or recent SARS-CoV-2 infection and exclusion of other plausible diagnoses. It usually affects children > 7 years of age and disproportionately of African, Afro-Caribbean or Hispanic origin. Cardiovascular (coronary artery aneurysm) and neurological (headache, encephalopathy, stroke, and seizures) complications may occur. |
Conclusions and future directions
The multiorgan sequelae of COVID-19 beyond the acute phase of infection are increasingly appreciated as data and clinical experience in this expanded time period. Active and future research needed includes the identification and characterization of key clinical, serological, imaging and epidemiological features of COVID-19 in the acute, subacute and chronic phases of the disease, which will help us better understand the natural history and pathophysiology of this new disease.
Active and future clinical studies, including prospective cohorts and clinical trials, along with frequent review of emerging evidence by task forces and task forces, are critical to developing a robust database of knowledge and informing clinical research. clinical practice in this area.
Currently, healthcare professionals caring for survivors of acute COVID-19 have the key role of recognizing, carefully documenting, investigating and managing new or ongoing symptoms, as well as following up on specific organ complications that have developed. during acute illness. It is also imperative that physicians provide information in accessible formats, including clinical trials available for participation and additional resources such as patient advocacy and support groups.
Furthermore, it is clear that care for patients with COVID-19 does not end at the time of hospital discharge, and interdisciplinary cooperation is necessary for the comprehensive care of these patients in the outpatient setting.
As such, it is crucial that health systems and hospitals recognize the need to establish dedicated COVID-1974 clinics, where specialists from multiple disciplines can provide integrated care.
Prioritization of follow-up care may be considered for those at high risk for post-acute COVID-19, including those who had severe illness during acute COVID-19 and/or required care in an ICU, those most susceptible to complications (e.g. for example, the elderly, those with multiple organ comorbidities, those post-transplant, and those with a history of active cancer) and those with the greatest burden of persistent symptoms.
Given the global scale of this pandemic, it is evident that healthcare needs for patients with COVID-19 sequelae will continue to increase for the foreseeable future. Addressing this challenge will require leveraging existing outpatient infrastructure, developing scalable healthcare models, and integrating across disciplines to improve the mental and physical health of COVID-19 survivors in the long term.