Highlights
|
Study questions:
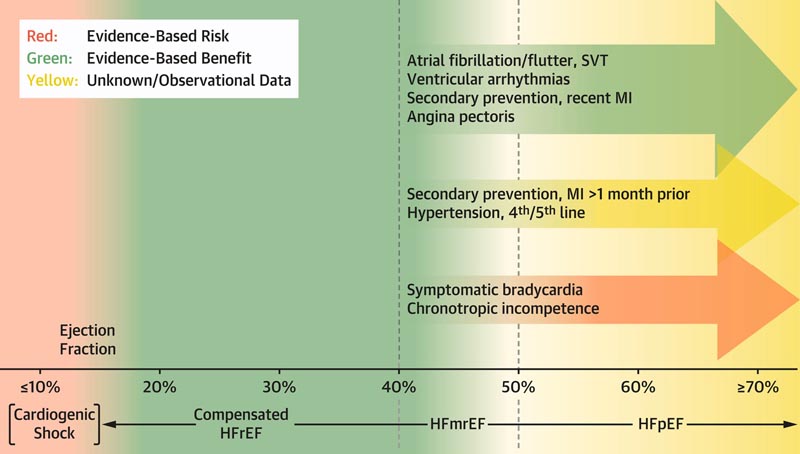
What is the association of beta blockers with hospitalization for heart failure (HF) and death in patients with HF and ejection fraction (EF) ≥ 40%?
Methods:
Investigators evaluated beta-blocker use at first encounter in outpatients ≥65 years of age with HF with mildly reduced EF (HFmrEF) and HF with preserved EF (HFpEF) in the United States PINNACLE Registry (2013-2017). .
Associations of beta-blockers with HF hospitalization, death, and the HF hospitalization/death composite were assessed using propensity score-adjusted multivariable Cox regression models, including interactions of EF × beta-blocker use.
Results:
Among 435,897 patients with HF and EF ≥40% (75,674 HFmrEF; 360,223 HFpEF), 289,377 (66.4%) were using a beta-blocker at first encounter; more commonly in patients with HFmrEF versus HFpEF (77.7% vs. 64.0%; p < 0.001).
There were significant interactions between EF × beta-blocker use for HF hospitalization, death, and the HF hospitalization/death composite (p < 0.001 for all), with increased risk with beta-blocker use as EF increased. .
Beta-blockers were associated with a lower risk of HF hospitalization and death in patients with HFmrEF, but with a lack of survival benefit and an increased risk of HF hospitalization in patients with HFpEF, particularly when EF was >60%.
Conclusions: The authors report that beta-blocker use was associated with an increased risk of HF hospitalization as EF increased, with a potential benefit in patients with HFmEF and a potential risk in patients with higher EF. |
Perspective:
This large observational study of patients ≥65 years with HF and LVEF ≥40% reports highly significant interactions between beta-blocker use and LVEF for both HF hospitalization and death, such that the risk associated with beta-blocker use increases as LVEF increases.
In patients with HFmrEF, beta-blockers appeared to be protective , but in patients with higher LVEF, particularly >60%, beta-blocker use was associated with no survival benefit and an increased risk of hospitalization for HF.
These data suggest caution with the use of beta blockers in patients with HFpEF due to a potentially increased risk of poor outcomes in these patients. Additional prospective trials are indicated to better understand the appropriate role and potential risks of beta-blockers in patients with heart failure and LVEF ≥40%.