Most episodes of diverticulitis are uncomplicated and can be safely treated conservatively without antibiotics or hospitalization. Although selected patients can be treated nonoperatively, perforated diverticulitis leading to peritonitis or a large abscess often requires surgical treatment. Surgical treatment usually consists of resection of the affected sigmoid colon and primary anastomosis (with or without a protective stoma ) or the Hartmann procedure (HP) with an end colostomy.
Since primary anastomosis carries a risk of anastomotic leak, especially when tissue healing has been compromised, for example by peritonitis, sepsis or ongoing chemotherapy, the Hartmann (HP) P procedure provides a safer operation. The downside of HP is the discontinuity of the colon and the need for another major reversal operation later or, alternatively, living with a permanent stoma.
Stoma reversal surgery (*) has been reported to carry a mortality rate of 0.4% to 5% and a morbidity rate of almost 50%. Previous studies have suggested that Hartmann colostomy after acute diverticulitis, or even after elective cancer resection with the intention of reversing the stoma, is not reversed in approximately one in three to four patients. These findings have created a vivid debate about the role of HP in the treatment of acute diverticular perforation.
Although recent randomized trials and guidelines have suggested sigmoid resection and primary anastomosis as a safe and preferable alternative to HP for perforated diverticulitis in hemodynamically stable patients without significant risk factors, HP will remain the method of choice for patients unstable and/or high risk.
Most studies on Hartmann colostomy reversal do not take into account the underlying disease leading to colon resection and include patients with colorectal cancer. Patients operated on for perforated diverticulitis comprise a significantly different patient population in terms of physical status and life expectancy compared to those operated on for malignant disease. Therefore, data from cohorts with mixed benign and malignant diseases as an indication for PH are of limited use to guide decision making considering patients with perforated diverticulitis.
The aim of this study was to investigate the rate of stoma reversal and the reasons for non-reversal in patients who had undergone HP due to acute diverticulitis. Additionally, complications related to stoma reversal and predictors of complicated recovery are reported.
Background
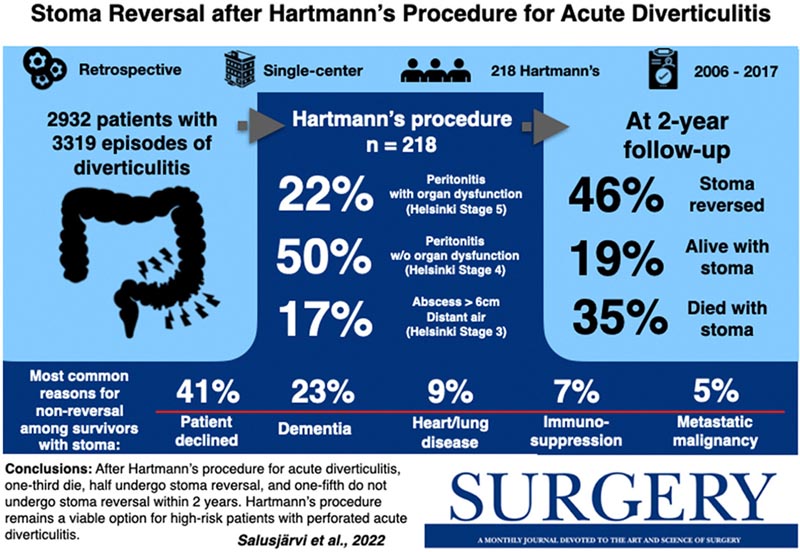
The Hartmann procedure is a treatment option for acute perforated diverticulitis, especially when organ dysfunctions exist. Its use has been criticized mainly due to fear of the high rate of permanent stomas. The aim of this study was to investigate the rate of stoma reversal, the reasons behind non-reversal, and the safety of reversal surgery.
Methods
This was a single-center retrospective study of patients undergoing urgent Hartmann procedure for acute diverticulitis between 2006 and 2017 with follow-up until March 2021.
Results
A total of 3,319 episodes of diverticulitis in 2,932 patients were examined. The Hartmann procedure was performed in 218 patients, of whom 157 (72%) had peritonitis (48 (22%) with organ dysfunction).
At 2 years, 76 (34.9%) patients had died with an ostomy , 42 (19.3%) were alive with an ostomy , and 100 (45.9%) had undergone stoma reversal . The survival of patients with and without reversal was 100% and 42.7% at 1 year, 96.0% and 35.0% at 2 years, and 88.9% and 20.7% at 5 years, respectively.
Risk factors for non-reversal were older age, need for outside assistance, low Helsinki staging for acute diverticulitis stage, and highest C-reactive protein level at hospital admission. The most common reasons for non-reversal in surviving patients were that the patient was unwilling to undergo the operation 18 (41%) and dementia 10 (23%).
Conclusion
After the Hartmann procedure for acute diverticulitis, one-third died, one-half underwent stoma reversal, and one-fifth did not undergo stoma reversal within 2 years.
Patients surviving with a stoma were either unwilling to undergo reversal or had severe comorbidities that preclude elective surgery.
The Hartmann procedure remains a viable option for high-risk patients with acute perforated diverticulitis.
Discussion
Several important findings regarding reversal surgery after HP for diverticulitis were observed in this study. First, only one-fifth of patients undergoing emergency HP were alive with a stoma 2 years after the initial operation. The rate was lower than that typically reported in previous series.
Second, the most common reasons for not undergoing reversal were patients who were not willing to undergo reversal operation and dementia.
Third, although 12% of patients had a major complication after reversal surgery, 90-day mortality was zero, demonstrating the safety of reversal surgery.
In summary , one-fifth of patients are left with a permanent stoma after HP for acute diverticulitis despite surviving long enough to undergo reversal. These patients are mostly high-risk older patients who require outside assistance in their daily routines.
In patients who underwent reversal surgery, the rate of major complications was relatively low (12%): 3% had an anastomotic leak, and mortality was 0%. HP remains a viable option for high-risk patients with acute perforated diverticulitis.
* The stoma is the artificial opening located in the abdomen to divert feces or urine to the outside.
Funding/Support: The study was funded by the Helsinki University Hospital Research Grants















