Background
Transfusion guidelines regarding platelet count thresholds before central venous catheter (CVC) placement offer conflicting recommendations due to a lack of good quality evidence. Routine use of ultrasound guidance has decreased CVC-related bleeding complications.
Methods
In a multicenter, randomized, controlled, noninferiority trial, we randomly assigned patients with severe thrombocytopenia (platelet count, 10,000 to 50,000 per cubic millimeter) who were being treated in the hematology ward or the intensive care unit to receive a prophylaxis unit platelet transfusion or no platelet transfusion before ultrasound-guided CVC placement.
The primary outcome was grade 2 to 4 catheter-related bleeding; a key secondary outcome was grade 3 or 4 bleeding. The noninferiority margin was an upper limit of the 90% confidence interval of 3.5 for the relative risk.
Results
We included 373 episodes of CVC placement involving 338 patients in the primary per-protocol analysis. Grade 2 to 4 catheter-related bleeding occurred in 9 of 188 patients (4.8%) in the transfusion group and in 22 of 185 patients (11.9%) in the nontransfusion group (relative risk, 2 .45; 90% confidence interval [CI], 1.27 to 4.70).
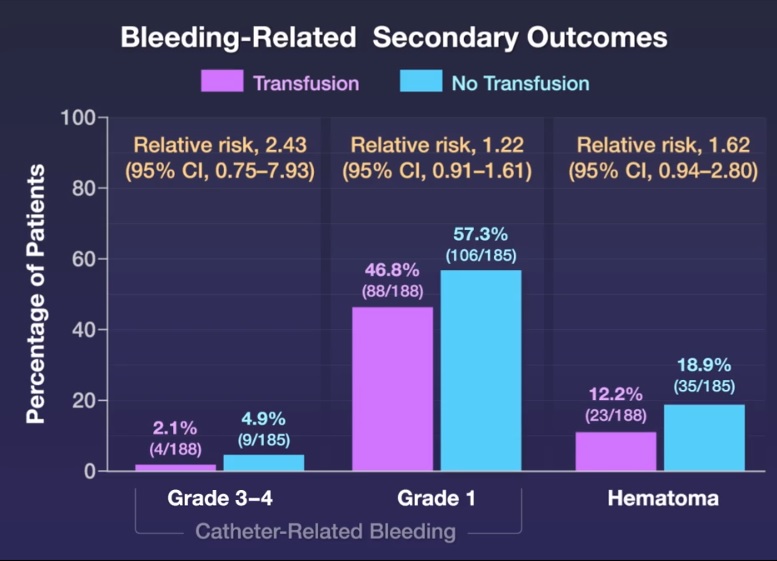
Grade 3 or 4 catheter-related bleeding occurred in 4 of 188 patients (2.1%) in the transfusion group and 9 of 185 patients (4.9%) in the non-transfusion group (relative risk, 2 .43; 95% CI, 0.75). to 7.93).
A total of 15 adverse events were observed ; of these events, 13 (all grade 3 catheter-related bleeds [4 in the transfusion group and 9 in the non-transfusion group]) were classified as serious.
The net savings of withholding prophylactic platelet transfusion before CVC placement was $410 per catheter placement.
Conclusions Withholding prophylactic platelet transfusion before CVC placement in patients with a platelet count of 10,000 to 50,000 per cubic millimeter did not meet the predefined noninferiority margin and resulted in more CVC-related bleeding events than transfusion of prophylactic platelets. |
(Funded by ZonMw; Dutch PACER trial registration number, NL5534. opens in new tab.)
Comments
Amsterdam UMC investigation shows bottom has been reached in restrictive blood transfusion policy
The trend in hospitals and guides is to be increasingly cautious with blood transfusions. Due to the associated side effects and the increasing scarcity and costs of blood products. For example, in recent years the number of patients receiving a transfusion during their stay in the ICU has been reduced by half. Researchers at the UMC Amsterdam, in collaboration with eight other Dutch hospitals, have shown that being increasingly restrictive in preventive blood transfusion is not, in all cases, understandable. The results of this study are published in the New England Journal of Medicine .
The research led by Amsterdam UMC is a collaboration between intensive care doctors and hematologists, who often face problems related to blood transfusion. One of these topics was the focus of the investigation. “In the ICU, more than half of patients receive a central venous catheter (CVC) for medication administration or dialysis. But what do you do when patients need a CVC and have a shortage of platelets , which causes clotting problems and increases the tendency to bleed? says lead researcher and head of the Amsterdam UMC Intensive Care Unit, Alexander Vlaar .
unexpected result
To prevent possible bleeding, the answer used to be a preventive platelet transfusion . In recent years, however, the question of whether a platelet transfusion is necessary to safely insert a catheter has been increasingly raised. The limit for which has also been halved in the last ten years, according to transfusion guidelines. “Therefore, we entered this study with the expectation that, as in other situations where this was already known, we could safely skip a platelet transfusion altogether. But the result was different. “Patients with very few platelets actually have less bleeding if they receive a transfusion before CVC placement,” adds Vlaar.
Stay critical
The researchers’ opinion is that the results of this study do not mean that all patients will have to undergo a transfusion from now on as a precautionary measure, but they do show that any possible cost savings should always be properly investigated. “If we had not further investigated this internationally implemented policy, doctors would simply follow this transfusion guidelines policy.
But we must remain critical here and, as physicians, continue to ask ourselves what risk we consider acceptable in cost reduction. In this study we show that we have to give a transfusion on average 14 times to avoid bleeding once. So the question is how much is bleeding prevention worth? That’s really a consideration that will have to be made every time,” says medical researcher Floor van Baarle.
A central venous catheter (CVC) is also often used in the treatment of hematological patients, but patients with hematological disorders have a completely different cause of low platelet count than patients in the Intensive Care Unit. “In hematology patients, platelet production is interrupted by the disease or chemotherapy, while most ICU patients produce platelets, but they are consumed immediately.
“Our study shows that placing a CVL without preemptive platelet transfusion as a precautionary measure leads to more bleeding in hematology patients than in ICU patients,” says principal investigator and hematologist Bart Biemond. “The good thing about this research project is the joint effort of two different disciplines, with patients and hematology and ICU doctors. “In this study, we show that cost-benefit assessment can work differently for different patients and that is very valuable.”















