Erythromelalgia (EM) is a rare debilitating disease characterized by episodes of burning pain associated with red, hot feet and occasionally hands.
During symptoms, the feet and hands may be swollen although edema is not universally present or reported.
Endogenous temperature control, probably through vasodilation of thermoregulatory arteriovenous anastomoses, may be a key factor in the pathophysiological mechanism of erythromelalgia (EM). Episodes are often triggered by physical activity and exposure to warm temperatures while the pain is typically relieved by cooling the affected areas.
Because symptoms are intermittent and the feet and hands may appear normal on presentation, the diagnosis may be missed. Patients often seek care from a variety of specialties, including primary care, dermatology, vascular medicine, neurology, and pain medicine. Patients have lower quality of life, increased morbidity and mortality as well as increased risk of suicide compared to the general US population.
Effective treatment to relieve symptoms is essential to avoid serious complications and improve outcomes. To name the condition, there are terms such as primary MS and secondary MS , but their use is varied and can lead to confusion.
Conventionally, the term secondary erythromelalgia is used for MS that has an identifiable underlying cause. The term primary MS is used for MS without an identifiable underlying cause (idiopathic MS). The term primary MS has also been used synonymously with inherited MS , to describe MS in patients with a family history of the disease. However, labeling MS as primary or secondary does not greatly affect its management.
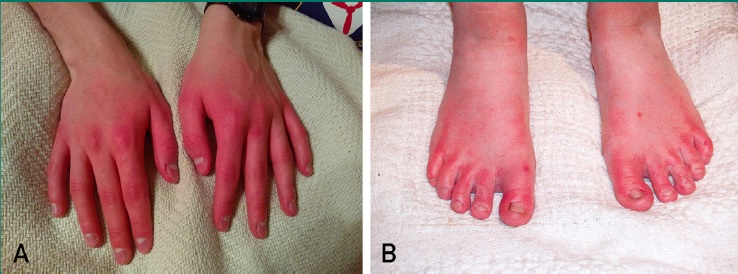
Hands and feet during an episode of erythromelalgia. The hands (A) and feet (B) may be red, painful, and hot.
| Primary erythromelalgia |
Approximately 5% of patients have a family history of MS, and many have an autosomal dominant inheritance.
In studies of families with autosomal dominant MS, a variant has been described in the sequence of the SCN9A gene, characterized by encoding the Nav1.7 subunit of neuronal sodium channels, located preferentially in the sympathetic ganglia and nociceptive sensory neurons of the ganglia. dorsal root.
The sequential variant, a gain-of-function variant, causes Nav1.7 neuronal sodium channels to open more easily and stay open, leading to multiple and prolonged activation in these sensory neurons. This helps explain the disproportionate pain patients experience during MS episodes. S has reported that this gain-of-function variant of Nav1.7 produces hypoexcitability of sympathetic neurons.
The natural history of primary MS has been well characterized from a relatively large series of 13 patients with primary MS and SCN9A sequence variants. Nearly a third of pain attacks had no identifiable trigger, and most patients had pain between attacks.
MS has been considered the first hereditary painful neuropathy known at the molecular level and as a disease model, which could be instructive for other painful conditions. However, familial MS is not always related to SCN9A. For example, a third-generation relative with primary MS had no SCN9A variants detected, suggesting that another gene could also be related to this disorder.
| Secondary erythromelalgia |
Many associations of MS with underlying disorders have been described, but it is not clear whether MS is truly secondary to these disorders. Approximately 5% of MS patients have a myeloproliferative disease (e.g., essential thrombocythemia and polycythemia rubra vera).
In these patients, management of the microvascular aspects of MS may be important, given that MS associated with a myeloproliferative disease is more likely to respond to aspirin .
Associations with underlying autoimmune diseases and other disorders as well as medications have been described, but are much less consistent.
| Association with neuropathy |
There is evidence of the close association between MS and small and large fiber neuropathy.
Almost 50% of MS patients show large fiber neuropathy on electromyogram and nerve conduction studies.
The presence of small fiber neuropathy is determined by functional evaluation of small fibers using sweat tests, including the sweat thermoregulation test and quantitative sudomotor axonal reflex testing.
Sweat thermoregulation testing shows marked abnormalities in approximately 90% of patients. This test is an excellent measure of small fiber sensory neuropathy in the skin, since sweat glands are mediated by small nerve fibers. Small fiber testing has also reported impaired small fiber function in MS patients.
Of note, findings on skin biopsy (often used to diagnose small fiber neuropathy) are typically nonspecific and show decreased epidermal nerve fiber density in only a minority of cases. Whether neuropathy leads to MS or vice versa is unclear. small fiber neuropathies could precipitate MS. Conversely, an underlying disease including Nav1.7 hyperexcitability and cold water treatment can also lead to small fiber neuropathy.
| Strategies for non-pharmacological management |
Symptoms of burning pain associated with episodes of redness of the extremities can dominate patients’ lives as they try to avoid situations that exacerbate their pain, and MS can progress to a debilitating chronic pain syndrome.
To help patients avoid this progression, they are advised not to abandon their usual lifestyle, seeking to avoid or minimize known triggers as much as possible. To do this, they should receive advice about lifestyle recommendations to minimize MS episodes and associated symptoms. These strategies are especially valuable because they can decrease the need for pharmacological and interventional treatments.
Patients should learn to control pain with topical and systemic medications; to address associated psychological problems, such as anxiety, and continue to exercise and participate in normal daily activities. These are all important techniques that help patients adapt to life with MS. There is no evidence that precipitating MS episodes, such as exercise, worsens the long-term outcome of the disease.
To relieve the pain of MS, patients often try to cool hot, red extremities with ice or cold water and continually use powerful fans near the extremities, but these actions can increase the risk of tissue damage, ulcerations, and disability. .
Water and ice can lead to immersion foot or trench foot , with swelling and ulceration of the skin. Wind can also cause injuries similar to burns, with exacerbation of flushing when the fans are stopped. Therefore, cooling measures to relieve symptoms must be safe.
The use of ice or water immersion should be avoided or limited (e.g., 10 minutes and 4 times/day), and patients should find alternative ways to cool their extremities. Some patients find relief by elevating the extremities during symptoms. Patients who have MS episodes with exercise, such as running, may be encouraged to try swimming.
| Pharmacological treatments |
MS is a difficult condition to treat. Topical and systemic treatments can be used. The results of the treatments are very variable. Many treatment reports were described several years ago (this literature review covers the years 1985-2021); There is little published data discussing the durability of the reported treatments.
Topical medications for relief of erythema and pain can be used as first-line treatment and may be all that is needed to manage this condition. For patients with secondary MS due to myeloproliferative disease, treatment should focus on addressing the underlying cause.
Aspirin is the first-line systemic treatment for patients with MS, particularly those who have underlying myeloproliferative diseases . Other systemic medications may then be considered.
Applying a multidisciplinary team approach is beneficial for the care of patients with MS. For patients who have severe, refractory, or disabled MS, referral to a comprehensive pain rehabilitation center is necessary.
| Topical treatments |
Topical treatments are considered a first-line pharmacological therapy for MS. They may be effective in suppressing pain or redness (or both), with decreased need for systemic medications, with fewer adverse effects compared to systemic medications.
Many topical treatments have been used for MS, with varying levels of effectiveness. Some treatments may be used to primarily address the pain associated with MS, while others may decrease redness with a subsequent decrease in pain. To evaluate the effectiveness of the topical medication, it should be used for at least 4 weeks before changing to another treatment.
> Topical pain therapy . Several topical medications have been used: lidocaine, amitriptyline combined with ketamine, and capsaicin.
> Lidocaine . It is an amide local anesthetic that blocks sodium channels required for neuronal impulse initiation and conduction, resulting in local anesthesia after topical application. It can be applied as a cream, ointment or patch to affected areas (feet, hands and other areas). Lidocaine patches are particularly practical to be applied to the dorsal or plantar surfaces of the foot, where up to 3 patches can be used for 12-24 hours. Patches may be more effective than cream or ointment because lidocaine is administered gradually over hours. In a series of 34 patients with MS presenting to a tertiary center, the majority who used 5% lidocaine patches saw improvement in pain, in contrast to 10 patients who did not respond to lidocaine gel. In that series, it was observed that all patients had tried several treatments before the lidocaine patch and that in general, patients with disease of greater severity and duration tended to have a lower response than to the lidocaine patch. No systemic absorption of lidocaine or symptoms of lidocaine toxicity were noted.
> Amitriptyline combined with ketamine. First described for use in MS in 2006, this topical combination in a vehicle, applied to affected areas up to 3 times/day, was useful in managing MS pain. Amitriptyline, a first-generation tricyclic antidepressant, inhibits the reuptake of serotonin and norepinephrine, and blocks sodium channels required for neuronal impulse initiation and conduction.
Ketamine is an antagonist of the N-methyl-D-aspartate receptor in peripheral terminals of primary nociceptive afferents; therefore, it also blocks neuronal impulses and may be effective in the dorsal root ganglia and dorsal horn. In a case series of 36 MS patients, 75% noted improvement in pain with topical 1-2% amitriptyline compounded with 0.5% ketamine. If this compound mixture is not effective, the ketamine concentration can be increased, as necessary, up to 5%. This combination needs to be prepared as a master recipe. In 2020, the US FDA granted orphan drug designation to a topical amitriptyline gel (ATX01; AlgoTx) as a treatment for MS.
> Capsaicin . Capsaicin may help control skin pain through desensitization of the TRPV1 receptor, leading to a decrease in the release of neurotransmitters such as substance P, an important chemical mediator in the transmission of pain impulses. There is little evidence to support the effectiveness of topical capsaicin in the treatment of MS. One case report noted that MS symptoms improved with topical application, 2 times/day, of 0.025% capsaicin cream. Two surveys noted that capsaicin was not helpful in most patients. In our own experience, capsaicin is not usually helpful for patients with MS. Topical capsaicin cream or lotion (0.025% to 0.075%) can be applied to affected areas, 3-4 times/day for 6 weeks, and patients should be warned that the medication may cause initial stinging and burning sensations. Topical capsaicin patches (0.025%) can be used off-label on affected areas as they are used for neuropathic pain associated with diabetic peripheral neuropathy of the feet; up to 4 topicals in a single 30-minute application, which can be repeated every 3 months as necessary but not more frequently. Theoretically, capsaicin patches can be used with a higher dose (8%), now for clinical use, for the treatment of chronic pain; It may be useful for the management of MS but its use in this disorder has not been well described.
> Other topical treatments . The strategies only have anecdotal evidence to support their use. For example, occasionally a mixture containing up to 5 ingredients may be used, adding topical formulations of ≥1 of the following to the amitriptyline-ketamine compound: clonidine, gabapentin, and lidocaine. Anecdotally, transdermal clonidine patches (0.1 to 0.3 mg/day) have been useful in reducing MS pain in some of the authors’ patients. They offer the advantage of weekly applications and, unlike lidocaine patches, can be placed anywhere on the body and not necessarily on the affected areas. Clonidine, an α2-adrenergic receptor agonist, may be useful in the treatment of MS by decreasing excess central sympathetic outflow through α2 receptors and peripherally counteracting aberrant vasoconstriction.
Other possible topical treatments include diclofenac 1% gel and gabapentin 6% ointment. Over-the-counter topicals containing camphor or menthol combined with methyl salicylate can help combat pain during MS episodes.
> Topical treatment for erythema. Vasoactive medications that cause vasoconstriction decrease redness during MS episodes. In some patients this results in a decrease in pain. Midodrine, an α1 agonist, used as a topical treatment may be useful. In a series of 12 patients, the use of midodrine 0.2% applied 3 times/day improved MS symptoms, including redness.
Other topical medications that have only anecdotal evidence to support their effectiveness may be helpful in reducing redness, such as topical oxymetazoline 0.05% and brimonidine tartrate 0.33%, applied daily (approved by the FDA for rosacea ) and 0.5% timolol maleate. Its continued use may cause erythema due to rebound effect.
> Systemic therapy. Special considerations . If topical treatments alone are not helpful, systemic treatments can be used. Aspirin may be useful, and should be tried in all patients who do not have contraindications.
> Aspirin . It is likely to be effective through its mechanism of inhibition of prostaglandin synthesis and platelet aggregation. It should be explored as a first-line systemic treatment for MS, given its low cost and relatively low adverse effect profile. For patients with MS who have no contraindications to aspirin, a daily dose of 325 mg is administered for at least 1 month. Aspirin is especially effective in patients who have secondary MS due to an underlying myeloproliferative disease, such as essential thrombocytosis and polycythemia vera. Dramatic improvement has been reported already in the first days of aspirin treatment. The antiplatelet effects of aspirin make it particularly useful in this subgroup of patients. In a series of 57 cases, Davis et al found that half of the patients reported that aspirin improved their symptoms, although other survey-based studies found no improvement in MS. Aspirin is the most common initial treatment for MS due to its overall safety, accessibility, and effectiveness, particularly in patients with myeloproliferative diseases.
> Other non-steroidal drugs. For patients who are allergic to aspirin, these drugs may be helpful. In the study by Davis et al, almost half of MS patients who tried ibuprofen, indomethacin, nabumetone, naproxen, or sulindac found the therapy somewhat or very helpful. Piroxicam has also been used successfully in the treatment of primary MS.
> Corticosteroids . Its systemic administration may be indicated in a subgroup of patients with MS, at the beginning of the disease course, before possible irreversible nociceptive remodeling and central sensitization occur. The mechanism of action of corticosteroids is believed to be to suppress any component of inflammatory neuropathy. Although the exact mechanisms of action are uncertain, corticosteroids may function as membrane stabilizers. A retrospective series of 31 cases identified a subgroup sensitive to corticosteroids among those who had a clear surgical, traumatic, or infectious precipitating diagnosis, and among those in whom the disease reached maximum intensity in less than 21 days. A corticosteroid trial may be warranted for many patients who have MS, regardless of age, particularly early in the course of the disease. However, not all patients respond to corticosteroids. For patients with MS who had a sudden or acute onset, a clear trigger, or a duration of less than 1 year, the authors recommend a therapeutic trial with systemic corticosteroids to evaluate their effectiveness. A regimen with a very high dose can be tried. The recommended dose is 1 g/day of methylprednisolone intravenously, for 3 consecutive days and then once/week for 11 weeks, or 1 g, once/week for 12 weeks. After a 12-week trial, the patient’s subjective and objective improvement should be evaluated. If the patient has evidence of improvement with this regimen, the use of corticosteroid-sparing immunosuppressive agents such as azathioprine and mycophenolate mofetil may be considered, with a gradual taper of systemic corticosteroids over 3 to 6 months. For a high-dose oral regimen, the authors recommend a daily dose of at least 40 mg of prednisone (or corticosteroid equivalent), 5 days, for a total of at least 200 mg of prednisone. A very high-dose regimen may be more effective than a high-dose regimen. More research is needed to explore the ideal dosage.
> Sodium channel blockers. These drugs have been investigated as a potential and promising treatment for MS, especially with the discovery that the sequence variant of the SCN9A gene that encodes the α subunit of voltage-gated sodium channels may be essential in the pathogenesis of MS. Primary hereditary MS (accounting for only about 5% of cases). Among neuropathic pain conditions, MS is the only one in which the sequential variant has been identified as causing the pain associated with this condition and therefore serves as a potential target. The sequential variant, a gain-of-function variant, causes Nav1.7 neuronal sodium channels to open more easily and remain open, resulting in repeated and prolonged neuronal activation in these sensory neurons. Even before the SCN9A variant was discovered, sodium channel blockers such as lidocaine and mexiletine had already been used to treat pain associated with MS and lidocaine may be effective. Mexiletine, a nonselective sodium channel antagonist, also functions as a class 1b antiarrhythmic. Mexiletine hydrochloride decreases the rate of rise of the action potential (phase 0) by inhibiting sodium influx current. In the study by Davis et al, 2 of 5 MS patients reported that mexiletine was somewhat helpful, while the others 3 did not find the treatment useful. In more recent in vitro and in vivo studies using animal models, mexiletine normalized the aberrant properties of the mutated Nav1.7 channels. 25 case reports have been found on the effectiveness of oral mexiletine in the primary treatment of MS, including in pediatric cases.
Carbamazepine, another oral agent with sodium channel blocking properties, has been reported to provide considerable pain relief, particularly in cases of MS with V400M variants in the SCN9A gene in both familial and de novo cases . Specifically, carbamazepine normalizes the activation of dorsal root ganglion cells that express Nav1.7 channels and attenuates the thermal hyperexcitability of these sensory neurons.
> Experimental studies of sodium channel blockers . A small, proof-of-concept, randomized, controlled trial found that an oral sodium channel blocker targeting the Nav1.7 sodium channel improves SCN9A-mediated MS pain symptoms. There are several new Nav1.7 sodium channel antagonists, including topical TV-45070 (also known as XEN402 and XPF-002) and oral PF-05089771) that may be promising therapies for primary MS in the future. , although these agents are undergoing trials and are not yet commercially available. A selective sodium channel blocker Nav1.7 pharmacologically reversed the phenotype induced by pluripotent stem cell-derived sensory neurons and blocked pain perception in patients with hereditary MS.
> Lidocaine infusion . Historically, lidocaine infusions have been used for acute pain syndromes. Examples of lidocaine infusions for acute MS pain control include use in an adult patient and a pediatric patient, both of whom were also transitioning to mexiletine. Lidocaine infusion regimens vary and include a weight-based bolus dose regimen of 1 to 2 mg/kg, a fixed bolus dose of 50 to 100 mg, and a continuous infusion of 1 mg/kg/hour. . The safety of lidocaine infusions is unclear, and neurological effects (slurred speech and mental status disturbances) are common. Therefore, intravenous lidocaine infusions are not currently recommended for MS. Mexiletine is a much safer oral alternative.
> Ketamine infusion . Ketamine infusions have been used to treat chronic pain syndromes at subanesthetic doses, with the added benefit of reducing opioid requirements. It has been described as a therapeutic option for a pediatric patient with MS. Ketamine can be used as an adjuvant analgesic therapy for MS. Some pain centers offer infusions with a combination of ketamine and lidocaine. Although some might consider a trial of ketamine infusion, the evidence supporting it is limited, and its use is controversial due to adverse effects and potential for abuse.
> Sodium nitroprusside . Infusions with sodium nitroprusside have been used in a subgroup of patients with MS and concomitant hypertension. Sodium nitroprusside interacts with oxyhemoglobin to produce nitric oxide, which ultimately leads to relaxation of vascular smooth muscle and lowering of blood pressure. Several case reports of pediatric patients with MS reported improvement in symptoms. However, in a survey by Cohen, MS symptoms worsened in an adult patient treated with sodium nitroprusside. While receiving this infusion, patients should be carefully monitored. The dose is gradually titrated to 2-4 mg/kg/minute. The evidence on the use of sodium nitroprusside is limited.
> Intravenous immunoglobulin . Intravenous immunoglobulin improved symptoms in 2 patients who had secondary MS, and may be considered for patients with autoimmune conditions. Therefore, the evidence for this use is limited.
> Antidepressants that inhibit serotonin and norepinephrine reuptake . These drugs have been used in the treatment of MS with variable success. It is believed that they affect vascular control and act on sympathetic fibers, inhibiting the reuptake of neuronal serotonin, norepinephrine and dopamine, and enhance the activity of neurotransmitters in the central nervous system (CNS). Among the drugs in this group, it is the most frequently used. In a pilot study of 10 patients, venlafaxine appeared to be relatively safe and an effective treatment for primary MS, with improvement in symptoms after the first week of treatment. Another study also reported that 2 out of 3 MS patients showed a response to venlafaxine. Sertraline has also been used, and in a study by members of the Erythromelalgia Association (TEA), symptoms improved in 6 of 9 patients treated with sertraline. However, fluoxetine, another selective serotonin reuptake inhibitor, induced MS in 1 patient. There are few data available for the use of duloxetine in the treatment of MS.
> Amitriptyline. The tricyclic antidepressant amitriptyline also inhibits the reuptake of serotonin and norepinephrine and also blocks sodium channels. The oral formulation was effective in the treatment of MS in a case report. The topical formulation has been combined with ketamine.
> Anticonvulsants.
Gabapentin and pregabalin . These two drugs have been used in the treatment of MS with variable success. Its use is frequent for the treatment of neuropathic pain, its effect is probably through binding to voltage-dependent calcium channels. Gabapentin is structurally related to the neurotransmitter gamma-aminobutyric acid. Gabapentin prevents allodynia and hyperalgesia in animal models, but the mechanism is not known. The conventional dosing regimen for initiating oral gabapentin is 300 mg 3 times/day, although alternative dosing regimens may be considered, and doses may be increased gradually to achieve the desired effect. In Cohen’s survey, a total of 16 patients reported improvement but none experienced remission. McGraw and Kosek also noted improvement in 2 MS patients who were treated with gabapentin. The medication is relatively safe; the most common adverse effect is sedation. The frequent occurrence of lower extremity edema has also been reported and may counteract the benefits provided by topical medications.
Pregabalin, a gamma-aminobutyric acid analog, may decrease neuropathic pain by binding to voltage-gated calcium channels in CNS tissue. Two cases were reported describing the improvement of MS with pregabalin. In one of the case reports, the patient had previously received a trial treatment with gabapentin without improvement, and was also using topical treatment.
> Prostaglandin and analogues . These medications have been useful in the management of MS due to their vasodilatory properties that decrease the microvascular arteriovenous shunt associated with MS.
> Iloprost (intravenous administration). It is a synthetic analogue of prostacyclin that dilates blood vessels and inhibits platelet activation. In a randomized, double-blind, parallel-group pilot study, 8 patients receiving intravenous iloprost had significantly fewer symptoms and less sympathetic dysfunction compared to 4 receiving placebo. Prostaglandin E1 and the synthetic prostacyclin analogue iloprost are administered by continuous infusions, so patients should be monitored closely.
> Misoprostol (oral administration). Misoprostol is an oral analogue of synthetic prostaglandin E1. In a double-blind, crossover study compared with placebo, orally administered misoprostol (0.4 to 0.8 mg/day) improved symptoms and decreased microvascular arteriovenous shunt compared with placebo. The beneficial effect of misoprostol is probably due to the decrease in microvascular arteriovenous shunting in the affected skin. In general, given the difficulty in obtaining the intravenous formulation of iloprost in the US, oral administration should be considered before opting for infusion.
> Calcium channel blockers. They include amlodipine, diltiazem and nifedipine, which have been used in MS with variable responses. Some authors suggest that these blockers may reduce hyperemia in MS by inhibiting vascular responses induced by α2-adrenoceptors. Davis et al reported that 85% of 20 MS patients who used vasodilators (diltiazem, nifedipine, and others) did not obtain any benefit. In an ASD survey, only 1 patient noted benefit from nifedipine, while the others had intolerable adverse effects (e.g., diarrhea), but 6 of 8 MS patients benefited from diltiazem, with near remission in 1 patient. . In contrast, there were cases in which calcium channel blockers induced MS. In the authors’ experience, calcium channel blockers can worsen MS while their discontinuation resulted in resolution of MS symptoms in several patients. Therefore, they generally do not recommend its use.
> Magnesium . Magnesium, both orally and in intravenous formulations, has been used in the treatment of MS due to its calcium channel blocking (and therefore vasodilatory) property. In an ASD survey, 8 of 13 patients treated with high doses of oral magnesium (600-6500 mg/day) had symptom improvement while in 1 patient, MS symptoms worsened. The author of this report recommends starting treatment with magnesium at the recommended daily dose (350 mg/day for women and 420 mg/day for men) to gradually increase, according to tolerance, because with the doses excessive, there is the possibility of gastrointestinal problems due to digestive intolerance, as well as muscle weakness, flushing, hypotension, bradycardia, blurred vision and cognitive effects. In the TEA survey, 2 patients had diarrhea when the dose was increased. In general, over-the-counter liquid or soluble magnesium products are better tolerated than tablets. Magnesium can also be administered intravenously every 2-3 weeks, at a dose of 2 g infused over 2 hours, but data describing the objective response to this regimen are limited.
> Antihistamines . They can be used but generally have limited value in the management of MS. Although MS does not appear to be a histamine-mediated disease, some researchers believe that a chronic local reaction may be involved, justifying its use. A case of a child with primary MS who partially improved with oral cetirizine hydrochloride has been reported. Cyproheptadine, an antihistamine and serotonin antagonist, was effective in relieving symptoms and hot skin in 2 patients with primary MS after they had failed to respond to other nonsteroidal anti-inflammatory drugs, including aspirin. However, in Cohen’s survey, none of the 3 patients benefited from its administration. Pizotifen, another antihistamine with serotonin antagonist activity, has been effective in the treatment of familial MS. In the aforementioned survey, 2 out of 3 TEA members benefited from antihistamine therapy. However, in a study by Davis et al, improvement occurred in less than a quarter of 28 patients who were prescribed antihistamines (cyproheptadine hydrochloride or diphenhydramine, phenylpropanolamine, trimeprazine, or cimetidine). Of all the antihistamines, cyproheptadine and pizotifen may be the most promising due to their additional property of blocking serotonin at serotonin receptors.
> Beta blockers . Limited data support the use of beta-blockers in patients with MS. In the study by Davis et al, most patients reported no benefit from these blockers (atenolol, nadolol, propranolol hydrochloride, or timolol), but occasionally patients reported a beneficial response. Their mechanisms of action in MS have not been established but it is believed that they decrease dose-related anesthetic-like membrane effects.
> Opioids . Although short-term use of opioids can help decrease the pain associated with MS, opioids are not considered a therapeutic option for MS, given the high risks, addictive potential, and need for long-term treatment.
> Other agents. Case reports have supported the use of several agents for MS, including ergotamine, sulodexide, pentoxifylline, busulfan, hydroxyurea, prazosin, quinine sulfate, ranolazine, carisoprodol, and pentazocine.
| epidural infusion |
Bupivacaine and ropivacaine are local anesthetics that decrease the hyperexitability of nociceptive fibers. Hyperexcitability and pain are decreased by reversible inhibition of voltage-gated sodium channels in nociceptive fibers of the trigeminal ganglia, dorsal root ganglia, and sympathetic fibers.
By interfering with the conduction of nociceptive fibers, epidural infusion with bupivacaine or ropivacaine can provide immediate pain relief, but it is often temporary. Although local anesthetics alone may provide benefits to MS patients, opioids such as fentanyl or morphine can be added for an additional analgesic effect.
Reports on the use of epidural infusions are scarce. There are reports of patients having longer pain relief. Of 11 patients who received epidural infusions for the treatment of refractory MS, 7 had a complete remission or were able to continue activities of daily living with minimal pain.
The remaining 4 patients also reported considerable pain relief, but additional interventions, such as a second epidural infusion and pharmacotherapy, were necessary in the long term.
At 30 months of follow-up, a second epidural infusion of bupivacaine relieved all symptoms in 1 patient. Although a second epidural infusion may be beneficial, pharmacologic intervention (e.g., oxcarbazepine, pregabalin, or mexiletine) after the infusion may be just as effective. Therefore, before a second infusion, residual pain should be controlled with pharmacological treatment. “Our experience,” the authors say, “is limited with epidural infusions for the management of MS, but we have not observed long-term pain relief as has been described in published reports.”
| Sympathectomy |
Sympathectomy has been described in different reports. Some results have been successful but others have not.
| Care from a multidisciplinary team |
Patients often benefit from a multidisciplinary team approach that includes dermatology, neurology, vascular medicine, and pain medicine. A multidisciplinary approach may be especially useful for patients with severe disease. For patients with underlying myeloproliferative disease, collaboration with an oncohematologist is valuable in managing the underlying disorder.
In patients with small or large fiber neuropathy, the intervention of the neurologist is important. If patients have a chronic pain syndrome, the involvement of a pain team and a pain rehabilitation approach can be extremely helpful.
Patients with MS typically have a chronic pain syndrome with central sensitization.
The effects on their lives can be devastating, and they may seclude themselves in their homes and engage in extreme behaviors to avoid precipitating MS episodes. Some patients are wheelchair bound and generally disabled. For patients with refractory MS whose lives have been severely affected by MS, or who have had no response to other treatments, a multidisciplinary pain and rehabilitation program should be considered.
Comprehensive pain rehabilitation centers offer a team made up of doctors, psychologists, occupational therapists and physical therapists. There are several pain rehabilitation programs. According to the authors, “we offer a three-week day treatment program with physical therapy and occupational therapy. Physiotherapy is intended for body reconditioning and increasing tolerance to activities.
Functional and behavioral problems of concurrent morbidities are addressed. The use of pain relievers, especially opiates, may be reduced and discontinued. The authors report the results of these programs carried out at their institution, stating that they “improved the physical status and emotional functioning of patients with severe, persistent MS.” After participating in a 3-week pain rehabilitation program, a patient who was confined to a wheelchair due to MS was able to walk and resume an active lifestyle, including playing golf regularly, a benefit that lasted for years.
Final recommendations
|















