> Summary Amid the coronavirus disease 2019 (COVID-19) pandemic, a host of logical fallacies and cognitive biases have interfered with understanding the nuances and communicating evidence-based guidance. In particular, multiple false dilemmas have run rampant on social media with the pitfalls of black-and-white messaging and reductionist framing. In this article, we carefully review the evidence around five false dichotomies related to COVID-19: 1) Health and lives versus economy and livelihoods. 2) Indefinite lockdown versus unlimited reopening. 3) Symptomatic severe acute respiratory syndrome versus asymptomatic coronavirus 2 infection. 4) Droplet vs. Aerosol Transmission of SARS-CoV-2 5) Masks for all vs. not wearing masks. While we recognize that there is no unequivocal answer, we call for comprehensive messaging and tailored policies informed by science that take into account shades of gray, uncertainties, and social contexts. |
Scientists and policymakers are operating on “pandemic standard time ,” fighting not only to advance science and policy but also to counter the “infodemic” of misinformation about coronavirus disease 2019 (COVID-19). ).
In recent months, a host of logical fallacies and cognitive biases have interfered with understanding the nuances and communicating evidence-based guidance.
In particular, a number of false dilemmas have run rampant on social media with the pitfalls of black- and-white messaging . Opponents on both sides of these hot debates choose science to fit narratives that align with their preconceptions. In this article, we deconstruct five false dichotomies related to COVID-19 by carefully and comprehensively reviewing the evidence.
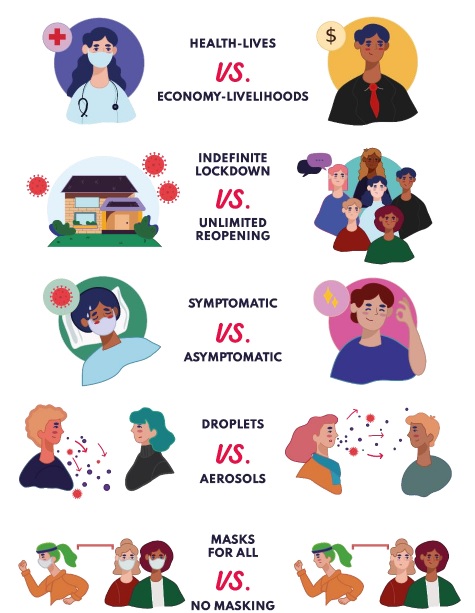
False dichotomies about COVID-19
| Health and lives versus economy and livelihoods |
A troubling dichotomy during the COVID-19 pandemic has been the idea that public health and the economy are two independent and opposing forces. That is, strategies implemented to protect public health necessarily harm the economic health of a nation. This dilemma has also been expanded to include civil health (i.e., the right to protest against public health measures such as lockdowns and threats to public health such as racism and police brutality) under the umbrella of economics.
There is no such dichotomy between public health and economics; In reality, they are intimately intertwined. The pandemic is an economic and public health crisis. The idea that the economy could function uninterrupted when a substantial proportion of workers suffer from an illness that may take weeks or months to recover from is idealistic at best.
Strong public health strategies that reduce the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) also protect the economy.
However, we should not ignore the physical and mental health effects and tremendous economic impact of COVID-19 or related countermeasures. Public health professionals, economists, and bioethicists must together evaluate trade-offs and develop proactive solutions to protect society’s multifaceted well-being.
For example, governments can consider freezing universal basic income and payments on rent and loans for all people, and paid leave for infected and exposed workers. More strategies are also needed to secure food supply chains, maintain essential outpatient healthcare services at normal performance, reduce unemployment, adapt businesses and minimize bankruptcies.
| Indefinite lockdown vs unlimited reopening (quarantine) |
Early in the pandemic, delays in the availability of testing and contact tracing prohibited reliance on isolating infectious people and quarantining their close contacts to slow the transmission of SARS-CoV-2. Governments were therefore forced to require all people to avoid non-essential contact by implementing stay-at-home orders, business and school closures, and travel restrictions.
These strict forms of physical distancing, although socially and economically devastating, were interim tools to limit the spread of SARS-CoV-2 in the early months of the pandemic while testing the infrastructure, contact tracing workforce, availability of personal protective equipment and hospital capacity were increased.
Currently, several countries and regions are reopening their economies to a greater or lesser extent. Premature opening without robust countermeasures can send societies back into lockdown, as illustrated by several US states that recently saw surges in COVID-19 cases following unrestricted reopening.
Rather than posing an all-or-nothing dilemma between remaining closed indefinitely and returning to pre-COVID-19 normality, economies can restart in a “new normal” scenario.
A progressive and cautious lifting of lockdowns and relaxation of other restrictions is only possible with non-pharmaceutical interventions that include expanded testing, rigorous contact tracing, isolation of infected individuals, and quarantine of exposed individuals. Given the imminent risk of a resurgence of COVID-19, plans are also needed to avoid overwhelmed health systems.
Since risk elimination is not feasible amid this pandemic, the right step is to advocate for a sustainable strategy like harm reduction . This requires education campaigns on SARS-CoV-2 transmission and assessment of personal exposure risk associated with routine activities, along with physical distancing, masks, respiratory etiquette, hand hygiene, environmental cleaning and disinfection, and improvement. of ventilation.
Shaming and stigmatizing people who violate preventive measures is likely to negatively reinforce risk behaviors rather than reduce them, and should be avoided. Lower-risk outdoor activities, staggered shifts, teleworking, and redesigning living and working spaces to avoid overcrowding and optimize ventilation are recommended to address quarantine fatigue and alleviate economic damage while that public health is protected.
| Symptomatic vs asymptomatic SARS-CoV-2 infection |
Seven months into the pandemic, confusion remains regarding asymptomatic SARS-CoV-2 infection, whether the proportion of people infected or the role of asymptomatic transmission. The issue of defining asymptomatic cases has been a challenge.
| Terminology : It is generally accepted that "asymptomatic" people do not show symptoms during the entire course of infection, "paucisymptomatic" or "oligosyptomatic" people have few or mild symptoms, and "presymptomatic" people do not show symptoms during the course of the infection. first days of infection but develop symptoms later. However, these terms continue to be misused to this day. |
Another complication is the wide clinical presentation of SARS-CoV-2 infection with symptoms such as fever, cough, shortness of breath, fatigue, myalgia, chills, rhinorrhea, sore throat, headache, anosmia, diarrhea, and dysgeusia.
The proportion of “asymptomatic” SARS-CoV-2-infected individuals has been variably reported from 4% to 96%; However, most of these cross-sectional point prevalence studies do not take into account the development of symptoms at a later date and overestimate the proportion of asymptomatic individuals.
Additionally, mild symptoms may not be determined by screening questionnaires or may not be remembered by patients. For example, it was established that 43% of participants in national screening in Iceland were asymptomatic, but how many of these patients were actually pre-symptomatic or pauci-symptomatic?
Other studies, such as a study from Vo, Italy, have reported a high prevalence of asymptomatic infection (43%), but symptoms narrowly defined as the presence of fever and/or cough. A preprint of a systematic review and meta-analysis estimated that only 15% (95% confidence interval: 10%-22%) of people infected with SARS-CoV-2 remain asymptomatic.
By taking more care to standardize symptom definitions , we can avoid misclassification errors and understand the true role of the COVID-19 presentation spectrum in driving the pandemic.
| Droplet vs aerosol transmission of SARS-CoV-2 |
COVID-19 has reawakened the long-standing debate over the dichotomous classification framework of respiratory droplets versus aerosols. Droplets and aerosols are mistakenly viewed as categorical modes of transmission rather than a continuum influenced by various aerodynamic factors such as particle size, emissions composition, turbulence, and ambient conditions.
- Large , heavier droplets (conventionally defined as >5 μm) typically settle quickly to the ground, remain airborne for short periods, and are generally transmitted over short distances, although airflow can propel them farther across a room.
- Small particle aerosols and droplet nuclei (<5 μm ) evaporate and disperse faster than they fall, remain suspended in air, and generally travel longer distances.
Unfortunately, confusion around the term "airborne" is due to the subtle difference between the normal meaning of the word (airborne) and scientific conventions that refer to aerosols or their speed of spread in the medium. atmosphere.
The risk of respiratory pathogen transmission varies with inoculum size, distance, duration, type of activity, environmental setting, and host factors.
While it is recognized that coughing, sneezing, talking, and breathing can generate both droplets and aerosols, there is ample evidence to support that SARS-CoV-2 infection occurs primarily, not exclusively, through larger droplets that reach the nose, mouth and eyes.
Contaminated fomites (contact transmission) and aerosols appear to play a minor role .
1. First, according to epidemiological studies, sustained person-to-person contact in crowded or unventilated spaces is an important factor in SARS-CoV-2 infection.
2. Second, the basic reproduction number (R0, 2-3) [18] and household secondary attack rates (generally 10% to 20%) for SARS-CoV-2 are consistent with the predominantly droplet transmission rather than aerosol transmission.
3. Third, hospital case and outbreak reports amid this pandemic have indicated that droplet and contact precautions work if applied in a timely and consistent manner, especially in the absence of aerosol-generating procedures (AGPs). .
Medical masks have been shown to reduce the infectious titers of other droplet-transmitted respiratory viruses, suggesting that any small unfiltered particles are less likely to contain infectious viruses.
Meta-analyses of studies comparing medical masks with filtering facepiece respirators (FFR) have reported no substantial differences in the prevention of respiratory viral infections (including seasonal coronaviruses and influenza) in healthcare workers. These data suggest that infectious aerosols do not predominantly occur during non-AGP healthcare, although the evidence is mixed and hampered by mask compliance.
In fact, there is no debate about whether a person infected with a respiratory pathogen can generate infectious aerosols. It is accepted that at least AGPs contribute to the spread of SARS-CoV-2 via aerosols, and experimental animal models and outbreak investigations suggest that short-range aerosol transmission may occur in situations of prolonged exposure in spaces unventilated interiors.
Furthermore, fomite transmission cannot be categorically excluded. Recently, the World Health Organization (WHO) has updated its guidance to recognize that, while airborne transmission of SARS-CoV-2 has not been demonstrated outside of AGPs and its extent remains unknown, the possibility cannot be ruled out. Simultaneous transmission by short-range aerosols. in favorable circumstances.
Despite evidence supporting droplets as the primary mode of transmission of SARS-CoV-2, narratives have emerged claiming that long-range aerosol transmission is a significant danger. These are based on studies of outbreaks in restaurants, telephone call centers, choirs, sports facilities, conference rooms, shopping malls, and bus transportation; studies demonstrating that experimentally generated SARS-CoV-2 aerosols remain infectious for up to 3 to 16 hours; evidence of viral RNA in air samples or hospital ventilation systems; evidence of viral RNA in outdoor particulate matter, and droplet dispersion models and experimental studies.
Epidemiological investigations could not exclude inhalation of droplets as the main mode of transmission. Although some air sampling studies have detected SARS-CoV-2 RNA, there is no evidence that the infectious virus persists in the air for long. In these studies and others that have failed to detect SARS-CoV-2 RNA, inconsistent findings could be related to sampling methodology, conditions, and infection prevention and control (ICP) measures.
Detection of viral RNA by reverse transcriptase polymerase chain reaction (PCR) is not equivalent to viral infectivity or viability.
Studies under controlled laboratory conditions showing the infectivity of aerosolized SARS-CoV-2 do not reflect normal host processes or real-world environmental conditions related to viral transmission. Furthermore, the transmission of small particles over long distances is especially subject to changes in ambient temperature, relative humidity, air flow, chemicals, and solar ultraviolet radiation that lead to dilution or inactivation.
While some respiratory particles can travel long distances or remain airborne for some time, the risk of transmission depends largely on the amount of infectious virus those particles contain. The lack of epidemiological and virological evidence supporting predominantly long-range aerosol transmission of SARS-CoV-2 suggests that infectious titers in small particles are insufficient to cause frequent infections.
There are unknown virological and biophysical characteristics of SARS-CoV-2 that are relevant to elucidate the modes of transmission, including the minimum infectious dose and airborne virus concentrations and the viability of the virus in natural indoor and outdoor environments based on the particle emission, size distribution, transformation, dispersion, deposition, time and environmental parameters. Currently available epidemiological data provide more reliable evidence of how SARS-CoV-2 spreads than laboratory, theoretical and in silico studies , especially if these do not investigate the infectivity of SARS-CoV-2 or are carried out in environments poorly simulated.
The transmission of infectious diseases has important implications for the development of effective preventive protocols and the allocation of resources. Exaggerated science can lead to harmful policies. For now, stating that aerosols are the dominant or exclusive mode of transmission of SARS-CoV-2 is reckless , as it would advance unnecessary IPC measures in hospital and community settings. Much more high-quality research is needed to prove otherwise.
Unfortunately, expanding on the results of studies with considerable methodological limitations, some mask advocates are even supporting the mass use of FFR in all healthcare areas and high-risk community settings. Conflicting messages regarding transmission routes may cause the public to be unwilling to comply with risk reduction practices.
For example, if the public mistakenly believes that transmission occurs mostly by virus-laden aerosols over a long distance and time, they may reject guidance to wear cloth masks given their limited aerosol-filtering capacity, or they may feel that distancing precautions are worthless.
Therefore, while SARS-CoV-2 transmission cannot be separated into the dichotomy of droplets versus aerosols, taking a confrontational stance against health authorities like the WHO and “aerosol scaremongering” is decidedly unhelpful . Aerosol scientists should work with health authorities, not against them.
| Masks for all vs not wearing masks |
Masking has sparked a culture war amid the COVID-19 pandemic.
On the one hand, some "pro-mask" academics and self-promoters have promoted masks with simplistic slogans such as "The science is simple and clear, masks are common sense, something is better than nothing" , inaccurate analogies with parachutes, and analysis and ecological fallacies without confounding control. Using inflammatory rhetoric, they have exaggerated the potential benefits and downplayed the potential unintended consequences.
On the other hand, there are two "anti-mask" groups : they strongly defend the principles of evidence-based medicine and therefore hope for "definitive" randomized clinical trials, and another that has strongly protested against masks based on claims unjustified (e.g., infringement on individual freedoms, increased risk of hypercapnia, clinical worsening of infected individuals). Unsurprisingly, deep-rooted conspiracy and scientific illiteracy have stoked anti-mask sentiment among the latter group.
Setting a binary choice between masks for everyone and no masks for anyone is misleading. More than a panacea or a hoax, masks are likely an effective prevention package component to combat the COVID-19 pandemic.
Masks, especially medical masks and FFRs, have been shown to prevent respiratory viral infections in healthcare. Regarding community settings, there is evidence of medical masks used by healthy and sick people in homes, university dormitories, schools, and the Hajj pilgrimage, but there is little research on cloth masks for source control. The vast majority of community and healthcare studies have focused on medical masks and FFRs, and have evaluated clinical and influenza-related outcomes.
Direct evidence of mask use related to coronavirus infections is scarce. Data on the filtration effectiveness of cloth masks has shown varying degrees of protection depending on the properties of the textiles, the number of layers, and facial fit. Mechanistic evidence has been published on the effectiveness of medical masks in reducing respiratory emissions of influenza virus and common cold coronavirus from symptomatic individuals.
Some observational studies of COVID-19 have suggested a benefit from community masking. In addition to a growing, albeit indirect and somewhat controversial, evidence base on the effectiveness of community masking in preventing viral respiratory infections, a critical concern underpinning masking during the COVID-19 pandemic has been the risk of involuntary transmission from individuals pre-symptomatic and asymptomatic, as demonstrated by contact investigations, modeling studies and virological studies.
All of these nuances explain the changes in recommendations from public health agencies in recent months as we move from the containment phase to the mitigation phase. Currently, several countries and regions with community transmission of SARS-CoV-2 recommend or require cloth masks and face coverings to mitigate its impact. However, from a public health standpoint, there are concerns about some policies and messaging about them.
The potential benefits of masks should be considered, but the potential disadvantages (i.e., shortages of medical and FFR masks for healthcare workers, cross-contamination due to improper mask use, complacency toward other masks) should not be completely ignored. preventive measures, social impact, environmental impact, psychological and physiological effects). Addressing these challenges may allow the potential benefits of masking to be maximized.
Inappropriate mask use is a persistent concern that points to failures in policy implementation, health education, community engagement, and research. Studies evaluating factors associated with public masking amid this pandemic may contribute to understanding potential barriers and designing strategies to increase mask compliance and acceptability.
Another concern with universal masking is that it is mandatory . Masking mandates, aimed at specific settings and situations, should come when their implications have been carefully considered. Widespread implementation of mandates can deepen social inequalities and erode public trust, especially in regions with no or low COVID-19 transmission.
Educational interventions should be preferred over coercive and punitive approaches (e.g., excessive fines, imprisonment, violence, stigmatization).
Governments imposing mass masking should ensure the availability of masks and consider distributing them to citizens free of charge. Public service providers could be mandated to have a stock of masks for users, and private companies could provide masks to customers out of self-interest.
Additionally, the impact on vulnerable populations needs to be addressed (e.g., hearing impaired people who rely on lip reading; racial groups asked to remove masks, harassed for hiding their face or are disproportionately penalized for not wearing masks; rural areas and poor populations without access to online educational tools).
Efficiency and effectiveness are not synonyms. There are still uncertainties surrounding the adoption of masking as a universal measure. COVID-19 research opportunities exist to obtain direct, actionable evidence. Gaps in research include the effectiveness of specific designs of cloth masks in high-risk community settings, the widespread use and reuse of cloth masks, the impact of different approaches to mask adoption, disadvantages of masks, attitudes and behaviors toward masks and the comparative effectiveness of cloth masks and face shields in the community.
It is enormously frustrating that academics who support masks but call for precise messaging and more testing are misrepresented as anti-mask and accused of malicious intent by some universal masking advocates. Undoubtedly, this pandemic demands effective communication of benefits, risks and uncertainties, as well as context-sensitive, data-driven policymaking that makes the case for and against interventions.
In line with the latest WHO guidance on masks, we advocate for a “smart” or risk-based community masking approach rather than a universal masking approach. Some exemptions for masking are reasonable. The term “universal” applies to people, places and times, without exceptions.
The dilemma of yes/no to masking must be replaced by a debate about who, where, when and how.
Some people really cannot or are contraindicated to wear a mask (e.g., people with some breathing difficulties, children under 2 years old), masking preschool children can be challenging and some people may prefer shields face masks, which likely offer advantages over masks in terms of eye protection,
no hand-to-hand contact, breathability, full-face visibility, scalable production, reuse and disinfection.
Likewise, not all environments and activities confer the same risk of infection. To improve the adoption of masking, policies should target risk contexts such as public gatherings, transportation, unventilated places, and confined environments, among others.
People engaging in activities of negligible risk (e.g., exercising in an uncrowded park while ensuring physical distancing, driving alone) should be exempt from wearing masks.
> Final observations
|
















