Background
As healthcare facilities begin to relax restrictions on healthcare services provided to patients (for example, restarting elective procedures), in accordance with guidance from local and state officials, there are precautions that must be maintained as part of the ongoing response to the COVID-19 pandemic.
Most of the recommendations in this updated guide are not new; They have been reorganized into the following sections:
- Best practices for routine healthcare during the pandemic.
- Recommended practices when caring for a patient with suspected or confirmed SARS-CoV-2 infection.
Best Infection Prevention and Control (IPC) Practices During the COVID-19 Pandemic
These practices are intended to apply to all patients, not just those with suspected or confirmed SARS-CoV-2 infection.
These additional practices include:
Implement telemedicine and nurse-led triage protocols
- Continue to use telemedicine strategies to provide high-quality patient care and reduce the risk of SARS-CoV-2 transmission in healthcare settings.
- When scheduling appointments for routine medical care (e.g., elective surgery), instruct patients to call ahead and discuss the need to reschedule their appointment if they have COVID-19 symptoms on the day they will be seen.
- If they do not have symptoms of COVID-19, advise them that they must still wear their face covering before entering the facility.
- If they do not have symptoms of COVID-19, advise them that they must still wear their face covering before entering the facility.
- When scheduling appointments for patients seeking evaluation for possible SARS-CoV-2 infection, use nurse-led triage protocols to determine if an appointment is necessary or if the patient can be cared for from home.
- If the patient must come in for an appointment, instruct them to call ahead to inform triage staff that they have symptoms of COVID-19 and to take appropriate preventive measures (e.g., follow triage procedures, wear face coverings with a mask before entering and throughout your visit or, if its use cannot be tolerated, holding a tissue against your mouth and nose to contain respiratory secretions).
Screening for signs and symptoms of COVID-19 in all those who enter a health center
Although symptom screening will not identify asymptomatic or pre-symptomatic individuals with SARS-CoV-2 infection, symptom screening remains an important strategy to identify those who might have COVID-19 so that precautions can be implemented. suitable.
- Take steps to ensure that everyone follows prevention measures and hand hygiene practices while in a healthcare facility.
- Post visual alerts (e.g., posters) at the entrance and in strategic locations (e.g., waiting rooms, elevators, cafeterias) to provide instructions (in appropriate language) on the use of a face covering or cloth face mask and how and when to wash your hands.
- Provide resources for respiratory hygiene and cough behavior, including 60-95% alcohol-based hand sanitizer, tissues, and disposal containers, at entrances to healthcare facilities, waiting rooms, and check-in. patients.
- Post visual alerts (e.g., posters) at the entrance and in strategic locations (e.g., waiting rooms, elevators, cafeterias) to provide instructions (in appropriate language) on the use of a face covering or cloth face mask and how and when to wash your hands.
- Limit and monitor entry points into facilities.
- Consider setting up screening stations outside the facility to screen people before they enter.
- Screen everyone (patients, healthcare professionals, visitors) entering the healthcare facility for symptoms consistent with COVID-19 or exposure to people with SARS-CoV-2 infection and ensure they are practicing pathway control. contagion.
- Actively take your temperature and document the absence of symptoms consistent with COVID-19. Fever is measured temperature ≥37.8° C or subjective fever.
- Ask them if they have been advised to quarantine due to exposure to someone with SARS-CoV-2 infection.
- Actively take your temperature and document the absence of symptoms consistent with COVID-19. Fever is measured temperature ≥37.8° C or subjective fever.
- Appropriately administer to anyone with symptoms of COVID-19 or who has been advised to self-isolate:
- Healthcare professionals should return home and notify occupational health services to arrange further assessment.
- Visitor access to the facilities must be restricted.
- Patients should be isolated in a room with the door closed.
- If a room is not immediately available, such patients should not wait among other patients.
- Identify a separate, well-ventilated space that allows waiting patients to be separated by 1.8 meters or more, with easy access to respiratory hygiene supplies.
- In some settings, patients may choose to wait in a personal vehicle or outside the healthcare facility, where they can be contacted by mobile phone when it is their turn to be evaluated.
- Depending on the level of transmission in the community, facilities may also consider designating a separate area in the facility (for example, an accessory building or temporary structure) or a nearby location as an evaluation area where patients with COVID-19 symptoms they can seek evaluation and care.
- Identify a separate, well-ventilated space that allows waiting patients to be separated by 1.8 meters or more, with easy access to respiratory hygiene supplies.
- Healthcare professionals should return home and notify occupational health services to arrange further assessment.
Reassess admitted patients for signs and symptoms of COVID-19
Although screening should be performed upon admission to the facility, it should also be incorporated into the daily evaluations of all admitted patients. Any fever and symptoms consistent with COVID-19 among patients should be managed and evaluated appropriately.
Implement universal protection measures
Source control refers to the use of cloth masks or face masks to cover a person’s mouth and nose to prevent the spread of respiratory secretions when they are talking, sneezing, or coughing.
Due to the potential for asymptomatic and pre-symptomatic transmission, control measures are recommended for everyone in a healthcare facility, even if they do not have COVID-19 symptoms.
- Patients and visitors should ideally wear their own cloth face covering (if tolerated) upon arrival and during their stay at the facility. If they do not have a face covering, they should be offered a face mask or cloth face covering, as supplies allow.
- Patients may remove the cloth face covering when they are in their rooms, but must put it back on when they are around other people (e.g., when visitors enter their room) or when they leave the room.
- Face masks and cloth face coverings should not be placed on young children under 2 years of age, on people who have trouble breathing, or on people who are unconscious, incapacitated, or otherwise unable to remove the mask without assistance.
- Patients may remove the cloth face covering when they are in their rooms, but must put it back on when they are around other people (e.g., when visitors enter their room) or when they leave the room.
- Healthcare professionals must wear a face mask at all times while in the healthcare facility, including in break rooms or other spaces where they may encounter co-workers .
- When available, face masks are preferred over cloth face coverings for healthcare professionals, as masks provide source control and protection for the wearer against exposure to splashes and aerosols of infectious material from others. .
- Cloth face coverings should NOT be used in place of a respirator or mask if more than source control is needed.
- Cloth face coverings should NOT be used in place of a respirator or mask if more than source control is needed.
- To reduce the number of times healthcare personnel must touch their faces and the potential risk of self-contamination, personnel should consider continuing to wear the same respirator or face mask (extended use) throughout their work shift.
- Respirators with an exhalation valve are not recommended for source control as they allow unfiltered exhaled breath to escape.
- Respirators with an exhalation valve are not recommended for source control as they allow unfiltered exhaled breath to escape.
- The health care professional must remove the respirator or face mask, perform hand hygiene, and put on a face mask when leaving the facility at the end of their shift.
- When available, face masks are preferred over cloth face coverings for healthcare professionals, as masks provide source control and protection for the wearer against exposure to splashes and aerosols of infectious material from others. .
- Educate patients, visitors, and healthcare professionals about the importance of performing hand hygiene immediately before and after any contact with their face mask or face covering.
Encourage physical distancing
The provision of healthcare requires close physical contact between patients and the healthcare professional. However, when possible, physical distancing is an important strategy to prevent the transmission of SARS-CoV-2.
Examples of how physical distancing can be implemented for patients include:
- Limit visitors to those essential to the patient’s physical or emotional well-being and care (e.g., caregiver, parent).
- Encourage the use of alternative mechanisms for patient and visitor interactions, such as video calling applications on cell phones or tablets.
- Schedule appointments to limit the number of patients in waiting rooms .
- Arrange seating in waiting rooms so that patients can sit at least 1.8 m apart.
- Replace in-person group activities (e.g., group therapy, recreational activities) by implementing virtual methods (e.g., video format for group therapy) or scheduling smaller in-person sessions, as long as patients sit at least 1, 8m away.
- In some circumstances, such as higher levels of community transmission or the number of COVID-19 patients cared for at the facility, and when healthcare-associated transmission occurs, facilities may cancel in-person group activities in favor of an exclusively virtual format.
For healthcare personnel, the potential for exposure to SARS-CoV-2 is not limited to direct patient care interactions. Transmission can also occur through unprotected exposures to asymptomatic or pre-symptomatic co-workers in break rooms or co-workers or visitors in other common areas. Examples of how physical distancing can be implemented include:
- Remind the healthcare professional that the potential for exposure to SARS-CoV-2 is not limited to direct patient care interactions.
- Emphasizing the importance of control of the source of transmission and physical distancing including areas where patients are not treated.
- Provide family gathering areas where all people (e.g. visitors, staff) can remain at least 1.8 m away from each other.
- Designate areas for staff to take breaks, eat and drink 1.8m apart, especially when they must remove face coverings.
Implement universal use of personal protective equipment
- Healthcare professionals working in facilities located in areas with moderate to high community transmission are more likely to encounter asymptomatic or pre-symptomatic patients with SARS-CoV-2 infection. If SARS-CoV-2 infection is not suspected in a patient presenting for medical care, the healthcare professional should follow standard precautions (and those based on transmission if necessary based on the suspected diagnosis).
-
- Wear eye protection in addition to a face mask to ensure that the eyes, nose, and mouth are protected from exposure to respiratory secretions during patient care.
- Wear an N95 or equivalent or higher level respirator, instead of a face mask, to:
- Aerosol generating procedures.
- Surgical procedures that could present a higher risk of transmission if the patient has COVID-19 (for example, those involving anatomical regions where viral loads may be higher, such as the nose and throat, oropharynx, respiratory tract).
- Aerosol generating procedures.
- Respirators with exhalation valves are not recommended for source control and should not be used during surgical procedures, as unfiltered expiration would compromise the sterile field.
- Wear eye protection in addition to a face mask to ensure that the eyes, nose, and mouth are protected from exposure to respiratory secretions during patient care.
- For healthcare professionals working in areas with minimal or no community transmission, the healthcare professional should continue to adhere to standard and transmission-based precautions, including the use of eye protection and/or an N95 respirator or equivalent or higher level based on anticipated exposures and suspected or confirmed diagnoses Universal use of face masks is recommended for healthcare professionals.
Consider targeted SARS-CoV-2 testing for patients without signs or symptoms of COVID-19
In addition to the use of universal PPE and source control in healthcare settings, specific SARS-CoV-2 testing can be used in patients without signs or symptoms of COVID-19 to identify those with asymptomatic or pre-infection. symptomatic SARS-CoV-2 and further reduce the risk of exposure in some healthcare settings.
Test results may lead to rescheduling of elective procedures or the need for additional precautions when caring for the patient. Limitations of using this testing strategy include obtaining negative results in patients during their incubation period who later become infectious and false negatives, depending on the testing method used.
Consider whether elective procedures, surgeries and non-urgent outpatient visits should be postponed in certain circumstances.
Facilities must balance the need to provide necessary services while minimizing risk to patients and healthcare staff. Facilities must consider the potential for patient harm if care for elective procedures, surgeries, and non-urgent outpatient visits is postponed.
Optimize the use of engineering and indoor air quality controls
- Optimize the use of controls to reduce or eliminate exposures by protecting professionals and other patients from infected people. For example:
- Physical barriers and special pathways to guide symptomatic patients through triage areas.
- Remote triage facilities for patient admission areas.
- Weather permitting, outdoor screening and triage stations for patients with respiratory symptoms.
- Vacuum rooms for surgical procedures that may generate aerosols.
- Reevaluate the use of open recovery areas.
- Physical barriers and special pathways to guide symptomatic patients through triage areas.
- Explore options to improve indoor air quality in all shared spaces.
- Optimize air treatment systems (ensuring directionality, filtration, rate of change, proper installation and regular maintenance).
- Consider adding portable solutions (e.g., portable HEPA filtration units) to increase air quality in areas where permanent air handling systems are not a feasible option.
- Optimize air treatment systems (ensuring directionality, filtration, rate of change, proper installation and regular maintenance).
Create a process to respond to SARS-CoV-2 exposures among staff and others
Health care facilities must have a process for reporting suspected or confirmed cases of SARS-CoV-2 infection, and must establish a plan, in consultation with local public health authorities, for how exposures will be investigated and managed in a facility. health facility. and how contact tracing will be carried out. The plan must address the following:
- Who is responsible for identifying contacts and notifying potentially exposed people?
- How will such notifications occur?
- What actions and follow-up are recommended for those who were exposed?
Contact tracing should be conducted in a manner that protects the confidentiality of affected individuals and is consistent with laws and regulations. Staff and patients who are currently admitted to the facility or have been transferred to another healthcare facility should receive priority for notification. These groups, if infected, have the potential to expose large numbers of individuals.
Healthcare facilities should be prepared for potential staffing shortages and have plans and processes in place to mitigate them, including providing resources to help healthcare professionals with anxiety and stress.
Recommended infection prevention and control practices when caring for patients with suspected or confirmed SARS-CoV-2 infection
Establish reporting within and between health centers and public health authorities
- Implement mechanisms and policies that promote situational awareness for health facility staff, including infection control, health care epidemiology, facility management, occupational health, clinical laboratory and frontline staff about patients with suspected or confirmed SARS-CoV-2 infection and facility response plans.
- Communicate and collaborate with public health authorities.
- Health care facilities should designate specific individuals within the facility who are responsible for communicating with public health officials and disseminating information to other staff.
Patient location
- For patients with COVID-19 or other respiratory infections, evaluate the need for hospitalization. If hospitalization is not necessary, home care is preferable if the individual’s situation allows it.
- If hospitalized, place the patient with suspected or confirmed SARS-CoV-2 infection in a single room with the door closed. The patient must have a dedicated bathroom.
- Negative pressure respiratory isolation rooms should be reserved for patients who will undergo aerosol-generating procedures.
- Negative pressure respiratory isolation rooms should be reserved for patients who will undergo aerosol-generating procedures.
- Staff entering the room must wear PPE.
- As a measure to limit staff exposure and preserve PPE, facilities could consider designating dedicated staff to exclusively care for patients with suspected or confirmed SARS-CoV-2 infection during their shift.
- Determine how staffing needs will be met as the number of patients with suspected or confirmed SARS-CoV-2 infection increases and/or if staff become ill.
- It may not be possible to distinguish patients who have COVID-19 from patients with other respiratory viruses. Patients with different respiratory pathogens can be grouped in the same unit. However, only patients with the same respiratory pathogen can be accommodated in the same room. For example, a patient with COVID-19 should ideally not be housed in the same room as a patient with an undiagnosed respiratory infection or a respiratory infection caused by a different pathogen.
- Determine how staffing needs will be met as the number of patients with suspected or confirmed SARS-CoV-2 infection increases and/or if staff become ill.
- To the extent possible, patients with suspected or confirmed SARS-CoV-2 infection should be housed in the same room for the duration of their stay at the healthcare facility (minimize room transfers).
- Limit transportation and movement of the patient outside the room to medically essential purposes.
- Whenever possible, perform procedures/tests in the patient’s room.
- Consider using portable x-ray equipment to reduce the need for patient transportation.
- Whenever possible, perform procedures/tests in the patient’s room.
- Communicate information about patients with suspected or confirmed SARS-CoV-2 infection to appropriate personnel before transferring them to other departments (e.g., radiology) and other healthcare facilities.
- Patients should wear a face mask or cloth covering to contain secretions during transport. If patients cannot tolerate a face mask or one is not available, they should use bandanas to cover their mouth and nose while outside their room.
- Once the patient has been discharged or transferred, staff should refrain from entering the unoccupied room until sufficient time has passed for sufficient air changes to remove potentially infectious particles. After this time has passed, the room must be properly cleaned and disinfected before being used again.
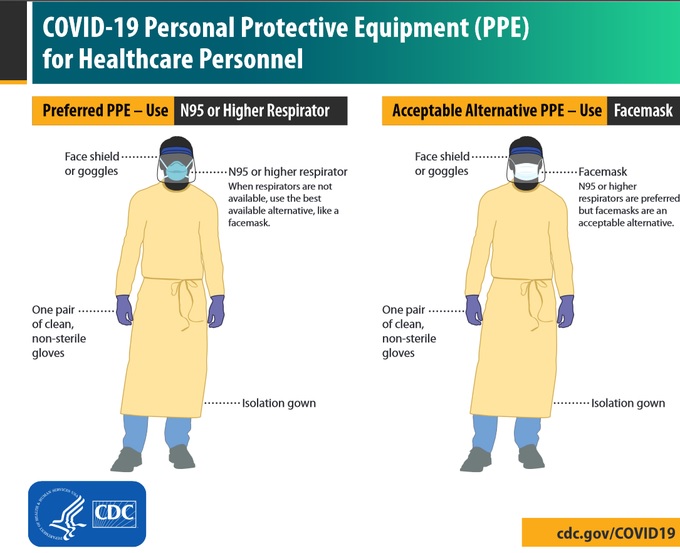
Personal protection equipment
Healthcare professionals entering the room of a patient with suspected or confirmed SARS-CoV-2 infection should follow standard precautions and wear an N95 respirator or equivalent or higher level respirator (or face mask if there is no respirator). respirator available), gown, gloves and eye protection.
When available, respirators (rather than masks) are preferred; They should be prioritized for situations where respiratory protection is most important and the care of patients with pathogens requiring airborne precautions (e.g., tuberculosis, measles, chickenpox).
- Hand hygiene
- Healthcare workers should sanitize their hands before and after all contact with the patient, contact with potentially infectious material, and before putting on and after taking off PPE, including gloves. Hand hygiene after removing PPE is particularly important to eliminate any pathogens that may have been transferred to bare hands during the removal process.
- Staff should sanitize their hands using a 60-95% alcohol solution or washing their hands with soap and water for at least 20 seconds. If hands are visibly dirty, use soap and water before the alcohol solution.
- Healthcare facilities must ensure that hand hygiene supplies are available to all staff at each care location.
- Healthcare workers should sanitize their hands before and after all contact with the patient, contact with potentially infectious material, and before putting on and after taking off PPE, including gloves. Hand hygiene after removing PPE is particularly important to eliminate any pathogens that may have been transferred to bare hands during the removal process.
- Training on personal protective equipment. Employers must select appropriate PPE and provide it to HCP in accordance with PPE standards. The PS must receive training and demonstrate understanding of:
- When to use PPE.
- What PPE is necessary.
- How to properly put on, use and remove PPE to avoid self-contamination.
- How to properly dispose or disinfect and maintain PPE
- The limitations of PPE.
Any reusable PPE must be properly cleaned, decontaminated and maintained after each use. Facilities should have policies and procedures that outline a recommended sequence for safely donning and doffing PPE.
Recommended PPE when caring for a patient with suspected or confirmed COVID-19 includes the following:
- Respirator or face mask (face masks or other cloth face coverings are NOT PPE and should not be used for patient care or other situations where the use of a respirator or face mask is recommended.]
- Put on an N95 respirator (or equivalent/superior respirator) or face mask (if you do not have a respirator) before entering the patient room or care area. Other respirators include other disposable filtering facepiece respirators, powered air-purifying respirators, etc.
- N95 respirators or respirators that offer a higher level of protection should be used instead of a face mask when performing aerosol-generating procedures.
- Disposable respirators and face masks should be removed and discarded after leaving the patient room or care area and closing the door. Clean your hands after removing your respirator or mask.
- If reusable respirators are used, they should also be removed after leaving the patient room or care area. They should be cleaned and disinfected according to the manufacturer’s reprocessing instructions before reuse.
- If reusable respirators are used, they should also be removed after leaving the patient room or care area. They should be cleaned and disinfected according to the manufacturer’s reprocessing instructions before reuse.
- Put on an N95 respirator (or equivalent/superior respirator) or face mask (if you do not have a respirator) before entering the patient room or care area. Other respirators include other disposable filtering facepiece respirators, powered air-purifying respirators, etc.
- Eye protection
- Put on eye protection (i.e., goggles or a face shield that covers the front and sides of the face) when entering the patient room or care area.
- Protective eyewear (e.g., safety glasses) with gaps between the glasses and the face probably will not protect the eyes from splashes and aerosols.
- Protective eyewear (e.g., safety glasses) with gaps between the glasses and the face probably will not protect the eyes from splashes and aerosols.
- Make sure the eye protection is compatible with the respirator so that it does not interfere with the proper positioning of the eye protection or the fit or seal of the respirator.
- Remove eye protection after leaving the patient room or care area unless implementing prolonged use.
- Reusable eye protection should be cleaned and disinfected before reuse. Disposable eye protection should be discarded after use unless protocols for extended use or reuse are followed.
- Put on eye protection (i.e., goggles or a face shield that covers the front and sides of the face) when entering the patient room or care area.
- Gloves
- Put on clean, non-sterile gloves when entering the patient room or care area.
- Change gloves if they are torn or heavily contaminated.
- Change gloves if they are torn or heavily contaminated.
- Remove and discard gloves before leaving the patient room or care area, and immediately wash your hands.
- Put on clean, non-sterile gloves when entering the patient room or care area.
- Outfit
- Put on a clean isolation gown or gown when entering the room or patient area. Change it if it gets dirty. Remove and dispose of in a dedicated waste or linen container before leaving the patient room or care area. Disposable ones should be discarded after use. If they are made of fabric, they must be washed after each use.
Aerosol generating procedures (AGP)
- Some procedures performed in patients with suspected or confirmed SARS-CoV-2 infection could generate infectious aerosols. Procedures that pose such a risk should be performed with caution and avoided if possible.
- If done, the following should occur:
- The health care professional in the room must wear an N95 or equivalent or higher level respirator, eye protection, gloves, and a gown.
- The number of professionals present during the procedure should be limited to only those essential for patient care and support of the procedure. Visitors should not be present at the procedure.
- AGPs should ideally take place in a negative pressure room.
- Clean and disinfect procedure room surfaces promptly.
- The health care professional in the room must wear an N95 or equivalent or higher level respirator, eye protection, gloves, and a gown.
Obtaining diagnostic samples
- When collecting respiratory diagnostic specimens (e.g., nasopharyngeal or nasal swab) from a patient with possible SARS-CoV-2 infection, the following should occur:
- Sample collection should take place in a regular examination room with the door closed.
- The healthcare professional in the room should wear an N95 respirator or equivalent or higher level respirator (or a face mask if a respirator is not available), eye protection, gloves, and a gown.
- If respirators are not readily available, they should be prioritized for other procedures with a higher risk of producing infectious aerosols (e.g., intubation). The number of people present during the procedure should be limited to only those essential for patient care and support of the procedure. Visitors should not be present for sample collection.
- Clean and disinfect procedure room surfaces promptly.
- Sample collection should take place in a regular examination room with the door closed.
Manage visitor access and movement within the facility
- Limit visitors in the medical facility to only those essential to the patient’s physical or emotional well-being and care (e.g., caregiver, parent).
- Encourage the use of alternative mechanisms for patient and visitor interactions, such as video calling applications on cell phones or tablets.
- If visits are made to patients with SARS-CoV-2 infection, visits should be scheduled and monitored to allow for the following:
- Health care facilities should assess the visitor’s health risk (e.g., whether the visitor has an underlying medical condition that puts them at higher risk for COVID-19) and the ability to comply with precautions.
- Healthcare facilities must provide instructions, before visitors enter patient rooms, on hand hygiene, limiting touched surfaces, and the use of PPE while in the patient room.
- Visitors should not be present during AGPs or other procedures.
- Visitors should be instructed to only visit the patient’s room. They should not go to other places in the health center.
- Health care facilities should assess the visitor’s health risk (e.g., whether the visitor has an underlying medical condition that puts them at higher risk for COVID-19) and the ability to comply with precautions.
Control of environmental infections
- Dedicated medical equipment should be used when caring for patients with suspected or confirmed SARS-CoV-2 infection.
- All non-proprietary, non-disposable medical equipment used for patient care must be cleaned and disinfected in accordance with the manufacturer’s instructions and facility policies.
- All non-proprietary, non-disposable medical equipment used for patient care must be cleaned and disinfected in accordance with the manufacturer’s instructions and facility policies.
- Ensure environmental cleaning and disinfection procedures are followed consistently and correctly.
- Routine cleaning and disinfection procedures are appropriate for SARS -CoV-2, including those patient care areas where aerosol-generating procedures are performed.
- Handling of clothing, food service utensils, and medical waste should also be done according to routine procedures.