1. The virus
SARS-CoV-2 contains more than 30,000 RNA bases. A proofreading mechanism prevents this large genome from accumulating frequent mutations. The large spike protein (S) forms a kind of crown on the surface of the viral particles. Its receptor-binding domain interacts with high affinity with angiotensin-converting enzyme 2 (ACE2) receptors on the surface of host cells.
After attachment, two host cell proteases (Furin and TMPRLRS) cleave the spike proteins and their exposed fusion peptides fuse the virus membrane with the host cell membrane. The virus’s RNA enters the cells of the upper and lower respiratory tract, and is translated into viral proteins. Other entry points are under investigation. The cell dies , releasing millions of new viruses that infect other cells and other individuals [1] .
2. The infection
There are several ways SARS-CoV-2 spreads. Infection begins with competition between SARS-CoV-2 virions that have reached the respiratory mucosa that express high levels of ACE2 receptors and the barrier created by mucus secreted by goblet cells and moved by hair-like cilia and immunity reactions. innate.
There is evidence of the presence of the virus in cells other than respiratory epithelia, including gastrointestinal epithelial cells, endothelial cells, and myeloid cells. We do not yet know how many SARS-CoV-2 are eliminated; However, the effectiveness of the first defense responses determines whether the infection will be benign or have serious consequences.
Figure 1 shows the selective determinants of susceptibility to COVID-19, including viral load, aging, lifestyle, and possibly genetics. If SARS-CoV-2 virions begin to replicate, they can reach and destroy cells in the lung alveoli and gastrointestinal tract. An immune overreaction ( cytokine storm ) can increase tissue damage [2, 3] 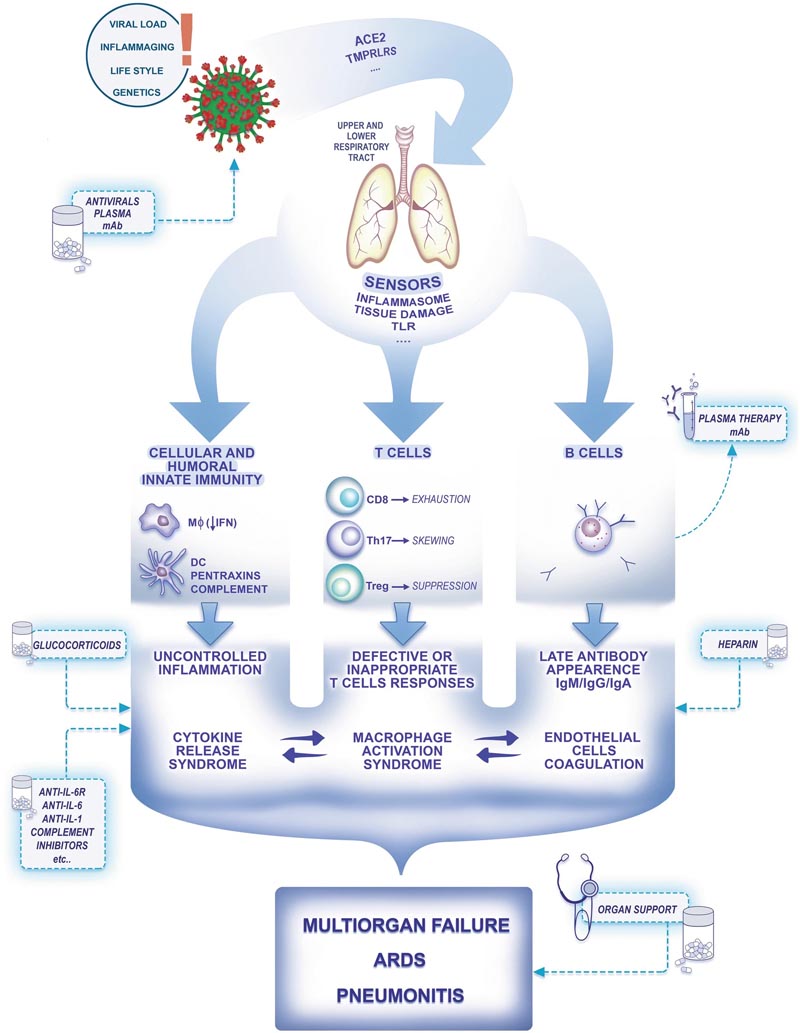
Figure 1: A schematic representation of the pathogenesis of COVID-19. ACE2, Angiotensin-converting enzyme 2, Toll-TLR receptors, M? macrophages, DC dendritic cells, Interferon IFN, Low arrow interferon Low IFN, Acute respiratory distress syndrome ARDS, dots indicate more receptors are involved (e.g. CD147 for viral entry).
3. Immunity
Innate cellular and humoral immunity represent a first line of resistance that is responsible for the majority of encounters with infectious agents. Evidence from SARS-CoV-1 suggests that these viruses may block interferon-mediated antiviral immunity (Fig. 1). Cytotoxic CD8 T cells play a critical role in antiviral resistance.
Evidence suggests that during COVID19 T cells experience functional exhaustion with lymphopenia , biasing towards a Th17 phenotype, inappropriate for antiviral immunity and suppression (Fig. 1) [4] . Antibody production occurs late after exposure (up to 20 days) and after the onset of symptoms (up to 15 days for 100% of patients with a positive score) [5] .
Interestingly, IgA antibodies are present in blood and saliva and may play a key role in immunity. There is evidence that symptomatic COVID-19 cases cause immunological memory and resistance to reinfection . According to SARS, immunological memory can be expected to last 2 to 3 years , a key aspect of immunity that needs to be defined.
4. Inflammation
Inflammation plays a key role in the development of COVID-19 from SARS-CoV-2 infection. Sensors of viral infection and cellular damage (e.g., inflammasomes; TLRs) trigger myeloid cell-dependent production of inflammatory cytokines (e.g., IL-1; IL-6; chemokines). Macrophages and inflammatory cytokines amplify local and systemic inflammation and are the main drivers of organ failure (Fig. 1).
While the role of inflammation in COVID-19 is obvious, it is unclear whether modulating the inflammatory response with drugs could bring benefits. Several drugs are currently being studied.
5. Thrombosis
As expected for a disease characterized by an inflammatory state in response to a viral infection, venous and arterial thromboembolic complications are common in hospitalized patients [6] . Microthrombi are present in the lungs, and alterations in the coagulation cascade can be measured at the systemic level. Endothelial dysfunction caused by both the direct cytopathic effect of the virus and the inflammatory reaction leads to a pro-thrombotic environment [3, 7] .
In hospitalized patients, there should be a low threshold to detect thromboembolic complications. On the other hand, more research is needed to look at the role of anticoagulation regimens versus standard thromboprophylaxis in the treatment of these patients [8] .
6. Diagnostic tests
The cornerstone of diagnostic testing is currently the evaluation of viral RNA in nasal or bronchoalveolar lavage samples by RT-PCR. Swab RT-PCR represents a bottleneck and hopefully saliva-based assays will address the urgent need for widespread testing.
More than 100 serological assays have been developed in industry or academic institutions, many of them poorly characterized. Given the timing and characteristics of the antibody response, properly validated assays are essential for epidemiological studies, evaluation of plasma donations, evaluation of memory and vaccine response, and as a complementary diagnostic in RT- PCR-negative patients.
There are no data available to show that a certain level of antibodies is associated with protection against subsequent exposure to SARS-CoV-2. Therefore, there is no reason for "immunity passports" or "immunity licenses" . A false perception of being “immune” can encourage irresponsible behavior [9] .
7. Clinical aspects
SARS-CoV-2 infection presents a variety of symptoms: it can be completely asymptomatic or present with severe symptoms. The incubation period of SARS-CoV-2 is 5.1 (4.5-5.8) days [10] . The prevalence of organ dysfunction varies. ARDS has been reported from as low as 3.4% to more than 10% of positive cases [3, 11, 12].
In Italy, while the country had the highest daily incidence of new cases, around 67% of patients showed mild symptoms and around 30% had symptoms requiring hospital admission. The most common symptoms are fever and cough . A small percentage of cases report gastrointestinal symptoms before the onset of respiratory symptoms.
Older patients with comorbidities are more likely to be severely affected and die. The most common reason for ICU admission is acute respiratory failure . Many patients developed severe ARDS. The involvement of other organs is often present.
8. Therapy
The mainstays of treatment are supportive therapy, respiratory support, and management of organ failure. Currently, there is no specific treatment for SARS-CoV-2 [13] . Chloroquine and hydroxychloroquine have been widely used; However, more and more evidence is emerging about its lack of effectiveness and possible harm .
Studies are currently evaluating the role of antivirals, steroids, and immunomodulatory therapies . Emerging evidence on the high incidence of arterial and venous thromboembolic complications is giving heparin a potential role in preventing these events.
Plasma from recovered patients has been used in China and elsewhere, including Italy, as a source of antibodies, as was done for SARS and MERS. Its safety and effectiveness in this disease have currently been studied.
9. Anti-SARS-CoV-2 vaccines
As we still do not know whether protection against COVID-19 is based on the action of antibodies or the activity of T cells, the implementation of approximately 150 programs for the development of vaccines based on different technological platforms is fully justified [ 14] .
To verify the effectiveness of the vaccine under “emergency use rules” , it has been proposed to vaccinate human volunteers and then intentionally challenge them. The WHO proposes prioritizing the effectiveness of the most promising vaccines in coordinated studies. Initially, it may not be physically possible to produce enough vaccines for the world’s population. However, the WHO is trying to ensure they are shared equitably, a crucial challenge.
10. Preparation and further research
If one thing is evident from the many deaths of this pandemic, it is that the world was not prepared from a structural, political, clinical and research point of view.
Several health workers have lost their lives. This is a very serious loss that no country can afford to repeat.
The two key principles that must be followed to control a potential surge in sick patients are to increase surge capacity and, more importantly, contain community transmission of the virus .
During an uncontrolled cluster, the volume of patients requiring ICU admission may be very high and efforts should be made to increase while ensuring the safety of non-COVID-19 patients and healthcare workers [15, 16] .
A wide range of therapeutic approaches have been tested under uncontrolled conditions. Today, like never before, we desperately need to recover the concepts of precision medicine that took decades to develop.
We must continue our efforts to bring the right treatment to the right patient at the right time. We shouldn’t look for a "magic bullet ," but we should praise efforts to answer research questions, and if the answer brings new questions, we should praise them even more.
The WHO SOLIDARITY trial or REMAP-CAP, an adaptively designed trial, is a promising way to answer some of these research questions [17] .
Photo by Javier Matheu on Unsplash