Highlights of the Declaration:
|
Summary
Diagnostic and therapeutic advances over the past decades have substantially improved the health outcomes of patients with acute coronary syndrome. Both age-related physiological changes and cumulative cardiovascular risk factors increase susceptibility to acute coronary syndrome throughout life. Compared with younger patients, acute coronary syndrome outcomes in the large and growing demographic of older adults are relatively worse.
Increased atherosclerotic plaque burden and anatomic disease complexity, combined with age-related comorbid cardiovascular and non-cardiovascular conditions, contribute to the poorer prognosis observed in older people. Geriatric syndromes, including frailty, multimorbidity, decline in cognitive and physical function, polypharmacy, and other complexities of care, can undermine the therapeutic efficacy of guideline-based treatments and also the resilience of adults. older people to survive and recover.
In this American Heart Association scientific statement, we (1) review the age-related physiologic changes that predispose to acute coronary syndrome and the complexity of management; (2) describe the influence of commonly encountered geriatric syndromes on cardiovascular disease outcomes; and (3) recommend age-appropriate and guideline-concordant acute coronary syndrome and revascularization management strategies, including transitions of care, use of cardiac rehabilitation, palliative care services, and holistic approaches. The primacy of individualized risk assessment and patient-centered care decision making is emphasized throughout.
The American Heart Association’s new Scientific Statements evaluate age-appropriate care for people 75 and older who are hospitalized and have heart attacks or chest pain.
Synthesis and Comments
According to a new scientific statement from the American Heart Association published in Circulation , the Association’s peer-reviewed flagship journal, for people aged 75 and older, age-related changes in overall health and in the heart and blood vessels must be taken into account and may require modifications in the way heart attacks and heart disease are treated.
The new statement, “Treatment of Acute Coronary Syndrome (ACS) in the Older Adult Population ,” highlights recent evidence to help physicians better care for patients aged 75 years and older. According to the statement, between 30% and 40% of people hospitalized due to ACS are 75 years old or older . ACS includes heart attacks and unstable angina (heart-related chest pain).
The statement is an update of the 2007 American Heart Association Statement on the Treatment of Heart Attacks in Older People.
Clinical practice guidelines are based on clinical trial research. “However, older adults are often excluded from clinical trials because their health care needs are more complex compared to younger patients,” said Abdulla A. Damluji, MD, Ph.D., FAHA, director. of the scientific statements writing committee, director of the Inova Center of Outcomes Research in Fairfax, Virginia, and associate professor of medicine at Johns Hopkins School of Medicine in Baltimore.
“Older patients have more pronounced anatomical changes and more severe functional impairment, and are also more likely to have health conditions unrelated to heart disease,” Damluji stated. “These include weakness, other chronic disorders (treated with various medications), physical dysfunction, cognitive impairment, or urinary incontinence, all of which are not routinely studied in the context of ACS.”
Normal cardiovascular aging and risk of acute coronary syndromes Age-related changes
Implications for acute coronary syndrome
|
Normal aging and age-related changes in the heart and blood vessels
Cardiovascular changes that occur with normal aging make ACS more likely to occur and can make diagnosis and treatment more complex: large arteries become stiffer; the heart muscle often works harder, but pumps less efficiently; blood vessels are less flexible and less able to respond to changes in the heart’s oxygen needs; and there is an increased tendency for blood clots to form.
Sensory impairment caused by aging can also alter hearing, vision, and pain sensations. Kidney function also deteriorates with age, causing more than a third of people over 65 to suffer from chronic kidney disease. These changes should be taken into account when diagnosing and treating ACS in older adults.
These considerations include the following points:
- ACS is more likely to present without chest pain in older adults and cause symptoms such as difficulty breathing, fainting, or sudden confusion.
- Measuring levels of the enzyme troponin in the blood is a standard test for diagnosing a heart attack in younger people. However, troponin levels may already be higher in older people, especially those with kidney disease and stiff heart muscle. Assessment of patterns of rise and fall in troponin levels may be more appropriate when used to diagnose heart attacks in older adults.
- Age-related changes in metabolism, weight, and muscle mass may require different anticoagulant medication options to reduce the risk of bleeding.
- As kidney function deteriorates, the risk of kidney injury increases, especially when contrast media are used in imaging tests and image-guided procedures.
- Although many doctors avoid cardiac rehabilitation in frail patients, they are often the ones who benefit the most.
- Ensuring continuation of medications and other therapies when transferring people from the hospital to an outpatient care facility is particularly important in older adults who are vulnerable to weakness, deterioration, and complications during these transitions.
Multiple medical conditions and medications
As people age, they are often diagnosed with health conditions that may worsen ACS or may complicate existing ACS. As these chronic conditions are treated, the number of medications prescribed may lead to unwanted interactions, or medications that treat one condition may worsen another.
“ Geriatric syndromes and the complexities of their care can undermine the effectiveness of ACS treatments, as well as the resilience of older adults to survive and recover,” Damluji said. “A thorough review of all medications, including supplements and over-the-counter medications, ideally with the advice of a pharmacist who has experience in geriatrics, is essential.”
An individualized, patient-centered approach to ACS care that considers comorbid conditions and the need for input from multiple specialists is best for older adults. Ideally, multidisciplinary teams caring for older adults with ACS include cardiologists, surgeons, geriatricians, primary care physicians, nutritionists, pharmacists, cardiac rehabilitation professionals, social workers, nurses, and family members.
Additionally, people with cognitive difficulties and limited mobility may benefit from a simplified medication schedule, with fewer doses per day and a 90-day supply of medications, so fewer refills are needed. Monitoring symptom burden, functional status, and quality of life during post-discharge follow-up are important to provide insight into how the patient is progressing relative to their goals of care and measure potential for improvement.
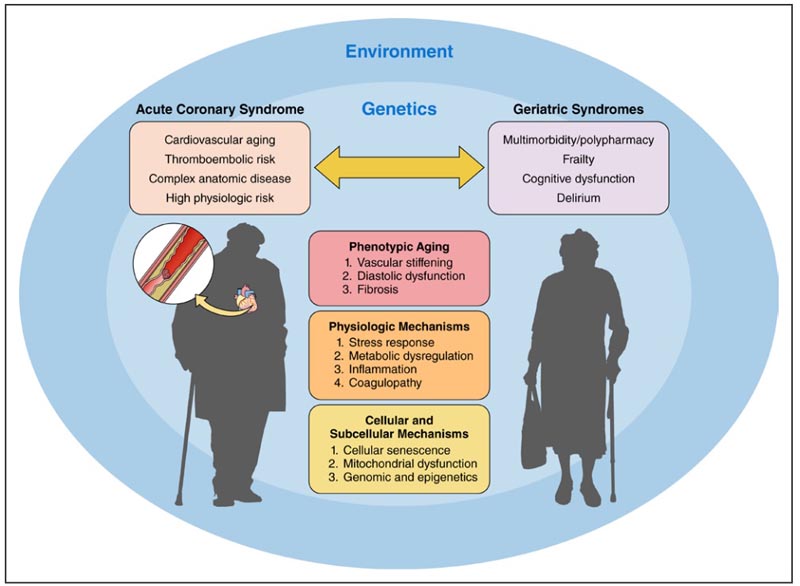
The bidirectional association between acute coronary syndrome and geriatric syndromes. Several factors influence this bidirectional association, including phenotypic aging, physiological mechanisms, cellular and subcellular mechanisms, genetics, and environment.
Patient preferences and life expectancy
Older adults differ widely in their independence, physical or cognitive limitations, life expectancy, and goals for the future. The goals of care for older people with ACS should go beyond clinical outcomes (such as bleeding, stroke, another heart attack, or the need to repeat procedures to reopen the arteries). Goals focused on quality of life, the ability to live independently, or return to previous lifestyle or living environment are important to consider when planning care for older adults with SCA. Additionally, do not resuscitate (DNR) orders should be discussed before any surgery or procedure.
- Although the risks are higher, surgical revascularization or procedures to reopen a blocked artery are beneficial options for older adults with ACS.
- If invasive treatment is chosen, a do-not-resuscitate (DNR) order may need to be suspended for the duration of the procedure.
- If invasive treatment is not chosen, palliative care can help control symptoms, improve quality of life, and provide psychosocial support.
- Important metrics for quality care include measurable goals, such as days patients spend at home and relief from pain and discomfort.
This scientific statement was prepared by the volunteer writing group on behalf of the Committee on Cardiovascular Diseases in Older Populations of the Council on Clinical Cardiology of the American Heart Association; the Cardiovascular and Stroke Nursing Council; the Council of Radiology and Cardiovascular Intervention; and the Council on Lifestyle and Cardiometabolic Health. The American Heart Association’s scientific statements promote greater awareness of cardiovascular disease and stroke problems and help facilitate informed health care decisions. Scientific statements describe what is currently known about a topic and the areas that need additional research. While these scientific statements inform the development of the guidelines, they do not constitute treatment recommendations. The American Heart Association guidelines provide the Association’s official clinical practice recommendations.
Co-authors are Vice President Daniel E. Forman, MD, FAHA; Tracy Y. Wang, MD, MHS, M.Sc., FAHA; Joanna Chikwe, MD, FAHA; Vijay Kunadian, MBBS, MD; Michael W. Rich, MD; Bessie A. Young, MD, MPH; Robert L. Page II, Pharm.D., MSPH, FAHA; Holli A. DeVon, Ph.D., RN, FAHA; and Karen P. Alexander, MD, FAHA. The authors’ statements are found in the article.
Download the complete document in PDF format in English here.