As of May 28, 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than 5.85 million people worldwide and caused more than 359,000 deaths . Emergency lockdowns have been initiated in countries around the world, and the effect on health, wellbeing, business and other aspects of daily life is being felt across societies and individuals.
With no effective pharmacological interventions or vaccines available in the imminent future, reducing the rate of infection (i.e., flattening the curve ) is a priority, and preventing infection is the best approach to achieve this goal.
SARS-CoV-2 spreads from person to person through close contact and causes COVID-19. It is unresolved whether SARS-CoV-2 could spread via aerosols from respiratory droplets; So far, air sampling has found virus RNA in some studies but not others. However, finding RNA viruses is not necessarily indicative of replication competent and infection competent (viable) viruses that could be transmissible.
The distance from a patient that the virus is infectious, and the optimal physical distance from person to person, is uncertain. For the currently foreseeable future (i.e., until a safe and effective vaccine or treatment is available), COVID-19 prevention will continue to rely on non-pharmaceutical interventions, including pandemic mitigation in community settings.
Therefore, quantitative assessment of physical distancing is relevant to inform the safe interaction and care of patients with SARS-CoV-2 in medical and non-medical care settings. The definition of close contact or potentially exposed helps with risk stratification, contact tracing, and developing guidance documents, but these definitions differ around the world.
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes COVID-19 and is transmitted from person to person through close contact. We aimed to investigate the effects of physical distancing, face masks, and eye protection on virus transmission in healthcare and non-medical (e.g., community) settings.
Methods
We did a systematic review and meta-analysis to investigate the optimal distance to prevent human-to-human transmission of the virus and to evaluate the use of face masks and eye protection to prevent virus transmission. We obtained data for SARS-CoV-2 and the betacoronaviruses that cause severe acute respiratory syndrome and Middle East respiratory syndrome from 21 WHO-specific and COVID-19-specific standard sources.
These data sources were searched from database inception to May 3, 2020, without restriction by language, for comparative studies and contextual factors of acceptability, feasibility, resource use, and equity. Records were examined, data extracted, and risk of bias assessed in duplicate.
We performed frequentist and Bayesian meta-analyses and random-effects meta-regressions. The certainty of the evidence was graded according to the Cochrane methods and the GRADE approach. This study is registered with PROSPERO, CRD42020177047.
Results
Our search identified 172 observational studies in 16 countries and six continents, with no randomized controlled trials and 44 relevant comparative studies in medical and non-medical care settings (n = 25,697 patients).
Virus transmission was lower with physical distancing of 1 m or more, compared with a distance of less than 1 m (n = 10,736, adjusted odds ratio [aOR] 0·18, 95% CI 0·09 a 0 · 38; risk difference [RD] −10 · 2%, 95% CI −11 · 5 to −7 · 5; moderate certainty); protection increased as the distance lengthened (change in relative risk [RR] 2·02 per m; pinteraction = 0·041; moderate certainty).
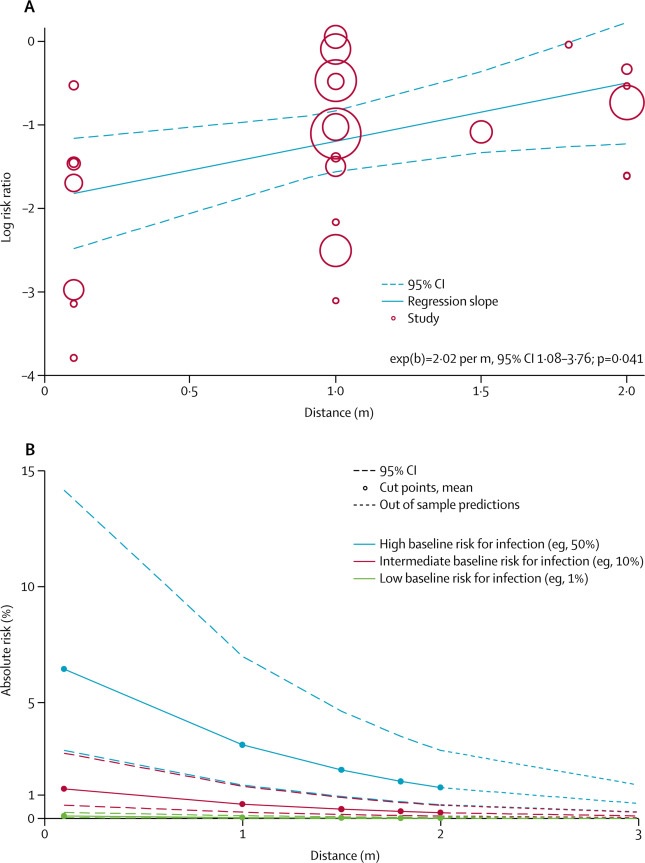 Change in relative and absolute risk with increasing distance
Change in relative and absolute risk with increasing distance
Wearing masks could result in a large reduction in the risk of infection (n = 2647; aOR 0 15, 95% CI 0 07 to 0 34, RD −14 3%, −15 9 to −10 7; low certainty), with stronger associations with N95 or similar respirators compared to disposable or similar surgical masks (e.g., 12-16-ply reusable cotton masks; pinteraction = 0 090; posterior probability > 95%, low certainty).
Eye protection was also associated with less infection (n = 3713; aOR 0 22, 95% CI 0 12 to 0 39, RD −10 6%, 95% CI −12 5 to −7 7; under certainty). Unadjusted studies and subgroup and sensitivity analyzes showed similar findings.
Interpretation
|
Discussion
The findings of this systematic review of 172 studies (44 comparative studies; n = 25,697 patients) in COVID-19, SARS and MERS provide the best available evidence that current physical distancing policies of at least 1 m are associated with a large reduction in infection, and distances of 2 m could be more effective.
These data also suggest that the use of face masks protects people (both healthcare workers and the general public) against infection with these coronaviruses, and that eye protection could confer an additional benefit.
However, none of these interventions provided complete protection against infection, and their optimal role may require risk assessment and several contextual considerations. No randomized trials were identified for these interventions in COVID-19, SARS or MERS.
Previous reviews are limited because they have not provided any evidence from COVID-19 or have not used direct evidence from other related emerging epidemic betacoronaviruses (e.g., SARS and MERS) to report the effects of interventions to reduce the current pandemic of COVID-19.
Previous data from randomized trials are primarily for common respiratory viruses such as seasonal influenza, with one systematic review concluding low certainty of the evidence to extrapolate these findings to COVID-19. Furthermore, previous syntheses of available randomized controlled trials have not accounted for cluster effects in analyses, leading to substantial imprecision in treatment effect estimates.
In between-study and within-study comparisons, we noted a larger effect of N95 or similar respirators compared to other masks. This finding is inconsistent with the conclusions of a review of four randomized trials in which low certainty of evidence was suggested for no major effect. However, in that review, the CIs were wide, so a significant protective effect could not be excluded. We harmonize these findings with Bayesian approaches, using proxy data from randomized trials to inform posterior estimates.
Despite this step, our findings continued to support the ideas not only that masks in general are associated with a large reduction in the risk of infection with SARS-CoV-2, SARS-CoV, and MERS-CoV, but also that N95 or similar respirators could be associated with a higher degree of protection against viral infection than disposable medical masks or multi-layer (12–16 layer) reusable cotton masks.
However, in view of the limitations of these data, we do not rate the certainty of the effect as high. Our findings are consistent with those of a cluster randomized trial showing a potential benefit of continuous use of N95 respirator over medical masks against seasonal viral infections.
More high-quality research is urgently needed, including randomized trials of optimal physical distancing and the effectiveness of different types of masks in the general population and for the protection of healthcare workers. Two trials were registered to better inform the optimal use of masks for COVID-19 (NCT04296643 [n = 576] and NCT04337541 [n = 6000]). Until such data are available, our findings represent the current best estimates for informing mask use to reduce COVID-19 infection.
We recognize that there are strong, perhaps opposing, feelings about policymaking during outbreaks. In one view, the 2007 SARS Commission report stated:
"...recognize, as an aspect of healthcare worker safety, the precautionary principle that reasonable action to reduce risk, such as the use of a tight-fitting N95 respirator, need not await scientific certainty."
"...if we don’t learn from SARS and get the government to fix the remaining problems, we will pay a terrible price in the next pandemic."
A contrary view is that scientific uncertainty and contextual considerations require a more nuanced approach. While challenging, policymakers should carefully consider these two insights along with our findings.
We found moderate certainty evidence that current policies of at least 1 m physical distancing are likely to be associated with a large reduction in infection, and that distances of 2 m could be more effective, as implemented in some countries. We also provide estimates for 3m. The main benefit of physical distancing measures is to prevent forward transmission and therefore reduce the adverse outcomes of SARS-CoV-2 infection.
Therefore, the results of our current review support the implementation of a physical distancing policy of at least 1 m and, if possible, 2 m or more. Our findings also provide robust estimates to inform modeling and contact tracing used to plan and strategize multi-level pandemic response efforts.
The use of face masks protected both healthcare workers and people in the community exposed to infection, and frequentist and Bayesian analyzes provided support for mask use regardless of setting.
Our unadjusted analyzes might, at first glance, suggest that face mask use in the community setting is less effective than in the healthcare setting, but after accounting for differential N95 respirator use between healthcare settings medical and non-medical, we detected no notable differences in the effectiveness of mask use between settings.
The credibility of effect modification in all settings was therefore low. Wearing masks was also acceptable and feasible. Policymakers at all levels should therefore strive to address equity implications for groups that currently have limited access to face masks and eye protection.
One concern is that mass mask-wearing could divert supplies from people most at risk of infection. Healthcare workers are increasingly being asked to ration and reuse PPE, leading to calls for government-led reuse of manufacturing capacity to overcome mask shortages84 and find solutions to mask use by the public in general. In this regard, some of the masks studied in our review were 12-16-ply reusable cotton or gauze masks.
At the moment, although there is a consensus that SARS-CoV-2 spreads mainly through large droplets and contact, debate continues about the role of aerosol, but our meta-analysis provides evidence (albeit of low certainty) that respirators They could have a stronger protective effect than surgical masks. Biological plausibility would be supported by data for aerosolized SARS-CoV-25 and preclinical data showing detection of seasonal coronavirus RNA in fine aerosols during tidal respiration, although, detection of RNA does not necessarily imply replication and competent virus. infection.
However, our findings suggest that it is possible that even in the absence of aerosolization , respirators could simply be more effective than masks at preventing infection. Currently, there is no data to support viable airborne viruses outside of aerosol-generating procedures from hospital studies available.
Other factors, such as superdiffusion events , subtype of healthcare setting (e.g., emergency room, intensive care unit, medical wards, dialysis center), whether aerosolization procedures are performed, and environmental factors such as ventilation, may affect the degree of protection provided by personal protection strategies, but we did not identify robust data to inform these aspects.
Strengths of our review include compliance with full systematic review methods, which included dual screening of titles and abstracts supported by artificial intelligence, full-text assessment, risk of bias assessment, and no language limitations. Patients infected with SARS-CoV-2, SARS-CoV or MERS-CoV were included and relevant data were searched up to May 3, 2020. We followed the GRADE16 approach to grade the certainty of the evidence. Finally, we identified and evaluated a large body of published work from China, from which much evidence emerged before the pandemic spread to other regions of the world.
Our comprehensive systematic review provides the best available information on three simple and common interventions to combat the immediate threat of COVID-19, while generating new evidence on drug treatments, vaccines, and other personal protection strategies.
|
Well-conducted, globally collaborative studies, including randomized trials, of different personal protection strategies are needed, regardless of the challenges, but this systematic evaluation of the best currently available evidence could be considered to inform interim guidance.
















