Background
Whether revascularization by percutaneous coronary intervention (PCI) can improve event-free survival and left ventricular function in patients with severe ischemic left ventricular systolic dysfunction, compared with optimal medical treatment (i.e., individually adjusted drug and device treatment for heart failure) alone, is unknown.
Methods
We randomly assigned patients with a left ventricular ejection fraction of 35% or less, extensive coronary artery disease amenable to PCI, and demonstrable myocardial viability to a strategy of PCI plus optimal medical therapy (PCI group) or optimal medical therapy alone (PCI group). medical-therapeutic group).
The primary composite outcome was death from any cause or hospitalization for heart failure. The main secondary outcomes were left ventricular ejection fraction at 6 and 12 months and quality of life scores.
Results
A total of 700 patients were randomized: 347 were assigned to the PCI group and 353 to the optimal medical therapy group.
Over a median of 41 months , a primary outcome event occurred in 129 patients (37.2%) in the PCI group and 134 patients (38.0%) in the optimal medical treatment group (hazard ratio, 0 .99; 95% confidence interval). [CI], 0.78 to 1.27; P=0.96).
Left ventricular ejection fraction was similar in the two groups at 6 months (mean difference, −1.6 percentage points; 95% CI, −3.7 to 0.5) and at 12 months (mean difference, means, 0.9 percentage points; 95% CI, −1.7 to 3.4).
Quality of life scores at 6 and 12 months appeared to favor the PCI group, but the difference had decreased by 24 months.
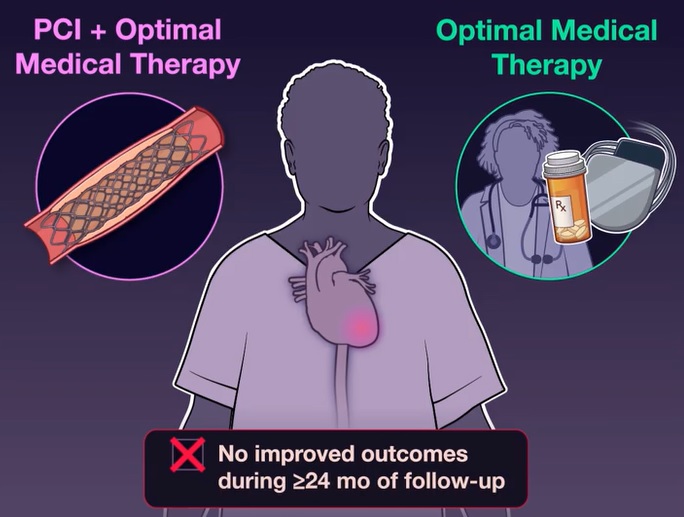
Conclusions Among patients with severe left ventricular ischemic systolic dysfunction who received optimal medical treatment, PCI revascularization did not result in a lower incidence of death from any cause or hospitalization for heart failure. |
(Funded by the Health Technology Assessment Program of the National Institute for Health and Care Research; REVIVED-BCIS2 ClinicalTrials.gov number, NCT01920048. opens in new tab.)
















