Under normal circumstances, the glomeruli filter only 0.008% of plasma albumin. Leakage across the glomerular membrane, caused by damage to (one of the layers of) the glomerular endothelial membrane, will cause more albumin to pass through the glomeruli, causing albuminuria . This is a disease mechanism that is well described in hypertensive and diabetic kidney disease and is generally related to intraglomerular hypertension.
In patients with chronic heart failure , the presence of albuminuria is a strong prognostic indicator of adverse events, such as mortality and hospitalization for heart failure, even after correction of diabetes, hypertension, and concomitant kidney disease. Although its prognostic value is well recognized, the underlying mechanisms of albuminuria in heart failure are not fully understood.
First, albuminuria could be a result of activation of the renin-angiotensin-aldosterone system (RAAS), since angiotensin can directly cause podocyte injury. Secondly, albuminuria could be the result of endothelial dysfunction, manifesting in both peripheral vessels and glomeruli. Third, albuminuria could be the result of increased renal venous pressure.
Two studies from the same group indicated that when renal venous pressure increased, albuminuria occurred, while external pressure on the renal parenchyma did not produce albuminuria. Finally, albuminuria could be an indicator of comorbidities that frequently occur with heart failure, such as diabetes and hypertension.
Furthermore, its differential relevance in heart failure with reduced (HFrEF) and preserved (HFpEF) ejection fraction has not been described. Therefore, we aimed to study the clinical characteristics and biomarker profile associated with albuminuria, in addition to the clinical outcomes described above, in patients with heart failure with both reduced and preserved ejection fraction.
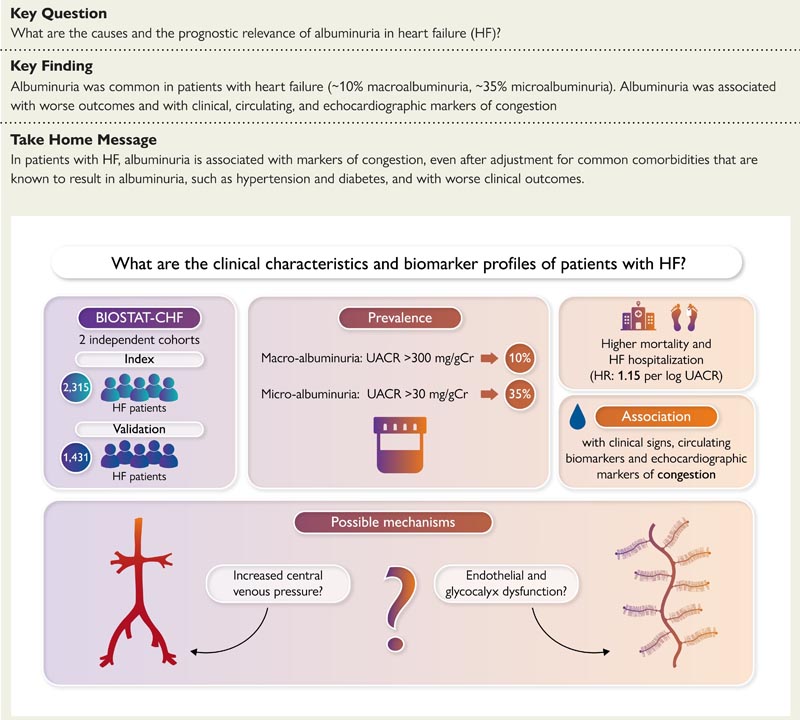
Graphic summary
Goals
Albuminuria is common in patients with heart failure and is associated with worse outcomes. The underlying pathophysiological mechanism of albuminuria in heart failure is still not completely understood. The association of clinical characteristics and biomarker profile with albuminuria was evaluated in heart failure patients with preserved and reduced ejection fractions.
Methods and results
Two thousand three hundred and fifteen patients included in the index cohort of BIOSTAT-CHF were evaluated and the findings were validated in the independent validation cohort of BIOSTAT-CHF (1431 patients).
Microalbuminuria and macroalbuminuria were defined as urinary albumin-creatinine ratio (UACR) >30 mg/gCr and >300 mg/gCr in urine samples, respectively. The prevalence of micro and macroalbuminuria was 35.4% and 10.0%, respectively.
Patients with albuminuria had more severe heart failure, as indicated by enrollment during admission, a higher New York Heart Association functional class , more clinical signs and symptoms of congestion, and higher concentrations of congestion-related biomarkers. such as biologically active adrenomedullin, cancer antigen 125, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) (all P < 0.001).
The presence of albuminuria was associated with a higher risk of mortality and (re)hospitalization for heart failure in both cohorts. The strongest independent association with log UACR was found for log NT-proBNP (standardized regression coefficient 0.438, 95% confidence interval 0.35–0.53, P < 0.001).
Hierarchical clustering analysis demonstrated that UACR clusters with markers of congestion and less clusters with indices of renal function. The validation cohort yielded similar findings.
Conclusion
In patients with new-onset or worsening heart failure, albuminuria is consistently associated with clinical, echocardiographic, and circulating biomarkers of congestion.
Discussion
The present study shows that heart failure patients who had albuminuria showed more signs and symptoms of (systemic) congestion at baseline compared to those who did not have albuminuria. Even after adjustment for several renal markers, such as urinary NGAL and KIM-1, the strongest association with log UACR was found for plasma NT-proBNP, in a multivariable regression analysis. Furthermore, the correlation between NT-proBNP and UACR was independent of glomerular filtration and remained present in all NYHA functional classes. Other markers and clinical parameters reflecting congestion, such as bio-ADM and peripheral edema, were also associated with higher UACR.
Finally, in hierarchical cluster analysis, UACR was grouped with new and established congestion markers, as well as the clinical congestion score, rather than with glomerular and tubular markers such as creatinine, NGAL, and KIM-1.
Taken together, these findings suggest that in patients with heart failure, the extent of albuminuria is more related to the severity of congestion than to markers of intrinsic kidney disease.
















