Although the predominant symptoms of COVID-19 are respiratory , gastrointestinal (GI) manifestations can occur and may be missed.
Enteric manifestations of SAR-CoV2 not only represent a major diagnostic challenge for clinicians when faced with patients with mild COVID-19 symptoms at initial presentation, but also signify possible fecal transmission of this virus.
With an increasing number of reported cases of COVID-19, there is a pressing need to systemically summarize the enteric manifestations of COVID-19 and the temporal pattern of fecal shedding of the SARS-CoV-2 virus, particularly to gastroenterologists and endoscopists who are not familiar. with this disease.
Methods
Researchers in Hong Kong evaluated clinical data from a cohort of COVID-19 patients and conducted a systematic review and meta-analysis of 60 studies with data on gastrointestinal symptoms (4,243 patients) and 11 with data on viral RNA in stool.
Results
- Among the 59 patients in the Hong Kong cohort (median age, 58), 25% had gastrointestinal symptoms, most commonly diarrhea and abdominal pain.
- Although all patients with gastrointestinal symptoms had fever , 54% did not have cough .
- Fecal viral RNA was positive in 15% of the 59 patients at presentation and in 9% of the 44 without gastrointestinal symptoms.
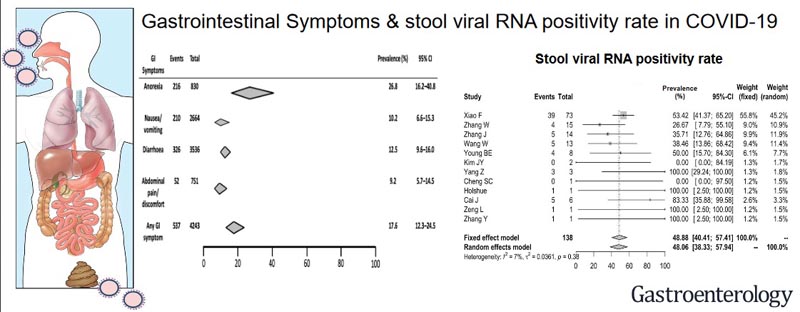
- In the meta-analysis, the combined prevalence of gastrointestinal manifestations was 18% .
- The most common symptom was anorexia (27%), followed by diarrhea (12%), nausea and vomiting (10%), and abdominal pain (9%).
- The prevalence of gastrointestinal symptoms was 17% in patients with severe disease compared with 12% in those with non-severe disease and was similar among adults, children, and pregnant women.
- The overall concomitant viral RNA positivity rate of stool and respiratory samples was 48%.
- In studies reporting serial testing, 70% of patients had persistently positive stool RNA even after respiratory tests became negative.
Discussion
In this meta-analysis of 4,243 COVID-19 patients from six countries , the combined prevalence of all gastrointestinal symptoms (including anorexia, nausea/vomiting, diarrhea, or abdominal pain) was 17.6% .
Anorexia was the most common gastrointestinal symptom (26.8%), followed by diarrhea (12.5%), nausea /vomiting (10.2%), and abdominal pain/discomfort (9.2%).
In the Hong Kong cohort, viral RNA was detected in the stool of 15.3% of patients at presentation, including patients without any gastrointestinal symptoms. Additionally, patients with diarrhea at presentation had higher stool RNA positivity and viral load than those without diarrhea.
We also noted that 48.1% of patients had detectable stool viral RNA during the course of the diseases. More importantly, prolonged shedding of viral RNA in feces rather than respiratory samples was observed in 70.3% of patients, which could be up to ≥33 days from disease onset.
Although diarrhea is one of the common gastrointestinal manifestations, the presence of constipation cannot rule out COVID-19, as a case report of four patients reported that constipation was observed in two.
Despite the inclusion of >60 reports, the true prevalence of any gastrointestinal symptoms might be underestimated as many previous studies did not report other gastrointestinal symptoms except diarrhea. Furthermore, most studies only reported gastrointestinal symptoms on the day of admission, but not throughout the course of the disease. The problem is further complicated by the difference in criteria for diagnosing diarrhea in various hospitals.
With more than 80% similarity to SARS-CoV, infection of the gastrointestinal tract by SARS-CoV-2 is not unexpected, and is proposed to be mediated by ACE2 cell receptors . ACE2 receptors are highly expressed in the small intestine, especially proximal and distal enterocytes, and the binding affinity of ACE2 receptors determines infectivity . As ACE2 modulates intestinal inflammation , SARS-CoV-2 can cause disruption of ACE2 function and lead to diarrhea.
A recent study demonstrated intracellular staining of viral nucleocapsid protein and ACE2 protein expression in human gastric, duodenal, and rectal epithelial cells, suggesting that ACE2 receptors could act as the entry point of the SARS-CoV-2 virus. CoV-2 in the intestinal tract.
Gastrointestinal manifestations were also commonly reported during the SARS and MERS outbreaks. In the previous SARS outbreak in Hong Kong, 16% of patients reported diarrhea. Similarly, up to a quarter of MERS patients also reported gastrointestinal symptoms such as diarrhea or abdominal pain. In our COVID-19 cohort in Hong Kong, 22% of patients reported diarrhea, which was slightly higher than our previous SARS cohort.
However, many of these patients came from a large outbreak during dinner on the Lunar New Year , who could contract the virus through the fecal-oral and respiratory routes , which partly explains the higher frequency of gastrointestinal manifestations.
Previous studies during SARS demonstrated that viral load in feces was strongly associated with the presence of diarrhea. In our COVID-19 cohort, patients with diarrhea also had a higher prevalence of detectable stool viral RNA at presentation.
Importantly, gastrointestinal manifestations may be the only initial symptoms in some patients with COVID-19. In the study by An et al, nine patients reported only gastrointestinal symptoms (predominantly anorexia [66.7%]) in the absence of fever or respiratory symptoms at presentation.
Another interesting feature of COVID-19 is recurrent infection in some patients, that is, recurrent symptoms after apparent recovery with respiratory samples positive for viral RNA again after initial clearance.
It remains to be determined whether the persistence of viral RNA in stool can be used as a surrogate monitor of recurrent infection in some patients.
Conclusions: In an analysis of data from the Hong Kong COVID-19 patient cohort and in a meta-analysis of publication results, we found that 17.6% of COVID-19 patients had gastrointestinal symptoms. Virus RNA was detected in stool samples from 48.1% of patients, including in stool collected after respiratory samples tested negative. Therefore, healthcare workers should exercise caution when collecting fecal samples or performing endoscopic procedures on patients with COVID-19, even during the patient’s recovery. |
Comment
A large number of studies now describe clinical experiences with COVID-19. Gastroenterologists and other clinicians should be aware that gastrointestinal symptoms are common (and may be the presenting manifestation) and that viral stool shedding occurs during the course of the disease (and may persist beyond this). Therefore, attention to prevent fecal-oral transmission of COVID-19 is crucial.