Dear editor,
In northern Italy, an overwhelming number of patients with Covid-19 pneumonia and acute respiratory failure have been admitted to our Intensive Care Units.
The focus is primarily on increasing the number of beds, ventilators, and intensivists dealing with the problem, while the clinical approach for these patients is that generally applied to severe ARDS , that is, high positive expiratory pressure ( PEEP) and prone positioning.
However, patients with Covid-19 pneumonia, who meet the Berlin criteria for ARDS, present an atypical form of the syndrome.
In fact, the main features we are seeing (confirmed by colleagues at other hospitals) is the dissociation between their relatively well-preserved lung mechanics and the severity of hypoxemia .
As shown in our first 16 patients (Figure 1), respiratory system compliance of 50.2 ± 14.3 ml/cmH2O is associated with a shunt fraction of 0.50 ± 0.11.
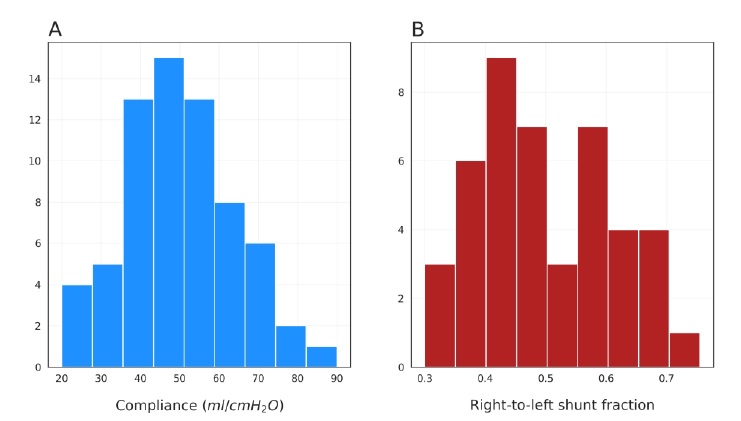
Such a wide discrepancy is virtually never seen in most forms of ARDS. The relatively high compliance indicates a well-preserved lung gas volume in this patient cohort, in stark contrast to expectations for severe ARDS.
| One possible explanation for the severe hypoxemia that occurs in compliant lungs is loss of lung perfusion regulation and hypoxic vasoconstriction. |
In fact, in ARDS, the ratio between the shunt fraction and the gasless tissue fraction is highly variable, with a mean of 1.25 ± 0.80 (1). However, in eight of our CT patients, we measured a ratio of 3.0 ± 2.1, suggesting notable hyperperfusion of gasless tissue.
If so, the increased oxygenation with high PEEP and/or prone position is not primarily due to recruitment, the usual mechanism in ARDS (2), but in these patients with poorly recruiting pneumonia (3), to the redistribution of perfusion in response to pressure and/or gravitational forces.
We should consider that: 1. In patients treated with continuous positive airway pressure or non-invasive ventilation, who present clinical signs of excessive inspiratory efforts, intubation should be prioritized to avoid excessive intrathoracic negative pressures and self-inflicted lung injuries (4). 2. High PEEP in a poorly recruiting lung tends to result in severe hemodynamic deterioration and fluid retention. 3. Prone positioning of patients with relatively high compliance results in modest benefit at the price of high demand on stressed human resources. |
After considering that, all we can do to ventilate these patients is to "buy time" with minimal additional harm: the lowest possible PEEP and gentle ventilation. We need to be patient.