Summary
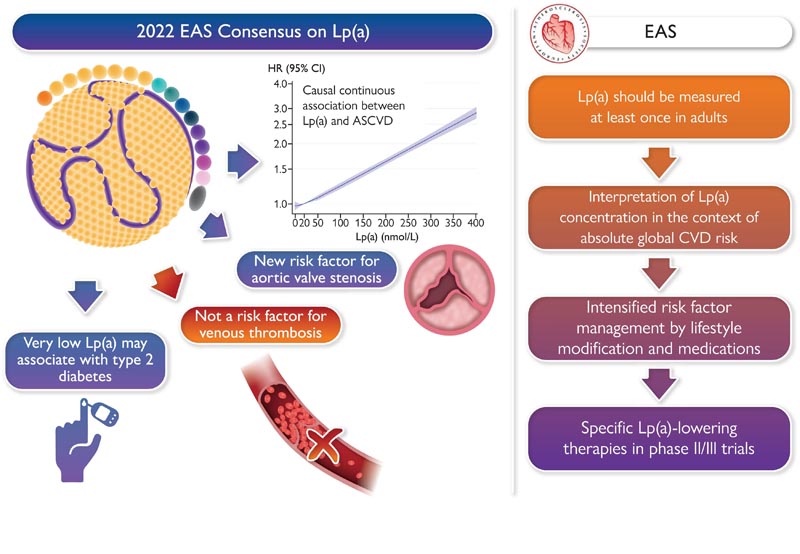
This 2022 European Atherosclerosis Society lipoprotein(a) [Lp(a)] consensus statement updates the evidence for the role of Lp(a) in atherosclerotic cardiovascular disease (ASCVD) and aortic valve stenosis, provides clinical guidance for testing and treating elevated Lp(a) and considers its inclusion in the overall risk estimate. Epidemiological and genetic studies involving hundreds of thousands of people strongly support a causal and continuous association between Lp(a) concentration and cardiovascular outcomes in different ethnicities; Elevated Lp(a) is a risk factor even with very low levels of low-density lipoprotein cholesterol. High Lp(a) is associated with both microcalcification and macrocalcification of the aortic valve.
The current findings do not support Lp(a) as a risk factor for venous thrombotic events and impaired fibrinolysis. Very low levels of Lp(a) may be associated with an increased risk of diabetes mellitus, which warrants further study. Lp(a) has proinflammatory and proatherosclerotic properties, which may be related in part to the oxidized phospholipids transported by Lp(a). This panel recommends testing Lp(a) concentration at least once in adults; cascade testing has potential value in familial hypercholesterolemia, or with a family or personal history of (very) high Lp(a) or premature ASCVD.
Without specific therapies to reduce Lp(a), early and intensive management of risk factors is recommended, directed according to overall cardiovascular risk and Lp(a) level. Lipoprotein apheresis is an option for very high Lp(a) with progressive cardiovascular disease despite optimal risk factor management.
In conclusion , this statement reinforces the evidence that Lp(a) is a causal risk factor for cardiovascular outcomes. Trials of specific treatments to lower Lp(a) are essential to confirm clinical benefit for cardiovascular disease and aortic valve stenosis.
Graphic summary
Key points from the 2022 Lp(a) consensus statement
Key points from the 2022 Lp(a) consensus statement. Current evidence demonstrates a continued causal association across ethnicities between Lp(a) concentration and cardiovascular outcomes, including aortic valve stenosis, but not for venous thrombotic events.
A meta-analysis of prospective studies shows that very low levels of Lp(a) are associated with an increased risk of diabetes mellitus. For clinical practice, Lp(a) should be measured at least once in adults and the results should be interpreted in the context of a patient’s absolute overall cardiovascular risk, with recommendations on early intensified control of risk factors through modification of lifestyle. The statement also reviews currently available and future possibilities to specifically reduce Lp(a).
Since the 2010 European Atherosclerosis Society (EAS) consensus statement, knowledge on the role of lipoprotein(a) [Lp(a)] in atherosclerotic cardiovascular disease (ASCVD) and stenosis has substantially expanded. aortic valve (AVS). The strong evidence for ASCVD causality prompted the development of new drugs that specifically reduce Lp(a) levels. New genetic, mechanistic, and imaging insights also suggest therapeutic potential in AVS, possibly the last major cardiovascular condition lacking medical therapy to slow disease progression. With the prevalence of AVS expected to increase dramatically (>300%) by 2050, this remains an urgent unmet clinical need.
What’s new since the 2010 EAS consensus statement?
|
Although it affects ≈1.4 billion people worldwide, 4 the contribution of elevated Lp(a) concentration to cardiovascular risk remains underappreciated. This second EAS statement highlights new evidence for Lp(a), identifies gaps that require further study, and provides clinical guidance for evaluating and treating elevated Lp(a) levels. This declaration should catalyze global action to improve Lp(a) management.
















