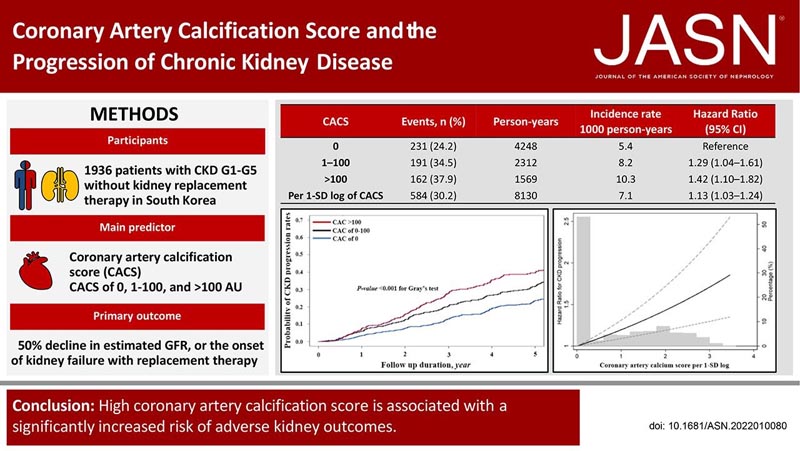
Highlights Coronary artery calcification (CAC) is an independent risk factor for cardiovascular disease (CVD) regardless of chronic kidney disease (CKD) status, and the CAC score (CACS) may have clinical implications beyond increased risk of CVD. In a prospective cohort study of 1936 CKD patients in South Korea, higher CACS (1–100 AU and >100 AU) was associated with a higher risk of CKD progression (1.29-fold and 1.42 times, respectively) compared with a CACS of 0. This association was consistent even after adjustment for nonfatal cardiovascular events treated as a covariate over time. Furthermore, the slope of eGFR decline was significantly greater in patients with higher CACS. These findings suggest that CACS may represent a potential risk for CKD progression and high odds of adverse CVD. |
Background
An elevated coronary artery calcification score (CACS) is associated with an increased risk of cardiovascular disease in patients with CKD. However, the relationship between CACS and CKD progression has not been elucidated.
Methods
We studied 1936 participants with CKD (stages G1-G5 without renal replacement therapy ) enrolled in the Korean Cohort Study for Outcome in CKD Patients. The primary predictor was Agatston CACS categories at baseline (0 AU, 1–100 AU, and >100 AU).
The primary outcome was CKD progression, defined as a ≥50% decrease in eGFR or development of renal failure on replacement therapy.
Results
During 8130 person-years of follow-up, the primary outcome occurred in 584 (30.2%) patients.
In the adjusted cause-specific risk model, CACS 1 to 100 AU (hazard ratio [HR], 1.29; 95% confidence interval [CI], 1.04 to 1.61) and CACS > 100 AU (HR, 1.42; 95% CI, 1.10 to 1.82) was associated with a significantly increased risk of the primary outcome.
The HR associated with recording 1 SD of CACS was 1.13 (95% CI, 1.03 to 1.24).
When nonfatal cardiovascular events were treated as a time-varying covariate, CACS of 1–100 AU (HR, 1.31; 95% CI, 1.07 to 1.60) and CACS >100 AU (HR, 1.46, 95% CI, 1.16 to 1.85) were also associated with an increased risk of CKD progression.
The association was stronger in older patients, those with type 2 diabetes, and those not using antiplatelet medications. It’s more,
Conclusion
Our findings suggest that high CACS is associated with a significantly increased risk of adverse renal outcomes and CKD progression.















