Effect of MRI-Guided Fibrosis Ablation Versus Conventional Catheter Ablation on Atrial Arrhythmia Recurrence in Patients With Persistent Atrial Fibrillation
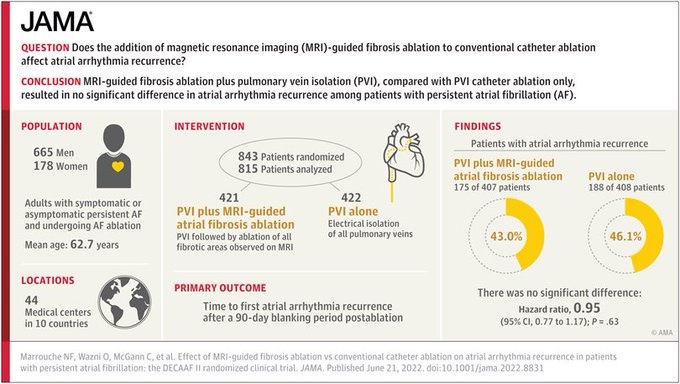
Key points Ask Among patients with persistent atrial fibrillation (AF), does the addition of magnetic resonance imaging (MRI)-guided fibrosis ablation to conventional catheter ablation affect atrial arrhythmia recurrence? Findings In this randomized clinical trial that included 843 patients with persistent AF, there was no significant difference in the recurrence of atrial arrhythmia in the MRI-guided fibrosis ablation group compared with the pulmonary vein isolation only group (ratio of risk, 0.95). Meaning The results do not support the use of MRI-guided fibrosis ablation for the treatment of persistent atrial fibrillation. |
Importance
Ablation of persistent atrial fibrillation (AF) remains a challenge. Left atrial fibrosis plays an important role in the pathophysiology of AF and has been associated with poor procedural outcomes.
Aim
To investigate the efficacy and adverse events of targeting atrial fibrosis detected on magnetic resonance imaging (MRI) to reduce recurrence of atrial arrhythmia in persistent AF.
Design, environment and participants
The Efficacy of Delayed Enhancement-MRI-Guided Fibrosis Ablation vs. Conventional Catheter Ablation of Atrial Fibrillation was a multicenter, investigator-initiated, randomized clinical trial involving 44 academic and non-academic centers in 10 countries.
A total of 843 patients with symptomatic or asymptomatic persistent AF and undergoing AF ablation were enrolled from July 2016 to January 2020, with follow-up until February 19, 2021.
Interventions
Patients with persistent AF were randomly assigned to pulmonary vein isolation (PVI) plus MRI-guided atrial fibrosis ablation (421 patients) or PVI alone (422 patients).
Late enhancement MRI was performed in both groups before the ablation procedure to evaluate baseline atrial fibrosis and 3 months after ablation to evaluate ablation scar.
Main results and measures
The primary endpoint was the time to first recurrence of atrial arrhythmia after a 90-day post-ablation blinding period.
The primary composite safety outcome was defined by the occurrence of one or more of the following events within 30 days of ablation: stroke, PV stenosis, hemorrhage, heart failure, or death.
Results
Among 843 patients who were randomized (mean age 62.7 years; 178 [21.1%] women), 815 (96.9%) completed the 90-day blinding period and contributed to the efficacy analyses.
There was no significant difference in atrial arrhythmia recurrence between groups (fibrosis-guided ablation plus PVI patients, 175 [43.0%] vs. PVI alone, 188 [46.1%]; hazard ratio [ HR], 0.95 [95% CI, 0.77]). -1.17], p = 0.63).
Patients in the fibrosis-guided ablation plus PVI group experienced a higher rate of safety outcomes (9 [2.2%] vs. 0 in the PVI group; P = .001).
Six patients (1.5%) in the fibrosis-guided ablation plus PVI group suffered an ischemic stroke compared with none in the PVI alone group.
Two deaths occurred in the fibrosis-guided ablation plus PVI group, and the first was possibly related to the procedure.
Conclusions and relevance
Among patients with persistent AF, MRI-guided fibrosis ablation plus PVI, compared with catheter ablation of PVI alone, produced no significant difference in atrial arrhythmia recurrence.
The results do not support the use of MRI-guided fibrosis ablation for the treatment of persistent AF.
ClinicalTrials.gov Trial Registration Identifier: NCT02529319















