NOTE: This preprint is currently available in the Journal of Heart and Lung Transplantation and is available to read now. Once it enters the testing stage, a citable digital object identifier (DOI) will be assigned to this document, which will be no later than March 25, 2020. See jhltonline.org for an updated version of this article.
The onslaught of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) 2019 (COVID-19) has gripped the world in a pandemic and challenged the culture, economy and health infrastructure of its population. It has become increasingly important for health systems and their clinicians to adopt a universal consolidated framework to recognize the staged progression of COVID-19 disease to deploy and investigate targeted therapy that is likely to save lives.
The largest COVID-19 report from the Chinese Centers for Disease Control and Prevention summarized findings from 72,314 cases and noted that while 81% were mild in nature with an overall case fatality rate of 2.3% , a small subgroup of 5% presented with respiratory failure, septic shock, and multiorgan dysfunction resulting in death in half of these cases, a finding that suggests that it is within this group that the opportunity to take life-saving action may be greatest. relevant.
Once the disease is evident, support measures begin with quarantines; however, a systematic disease-modifying therapeutic approach remains empirical.
Pharmacotherapy directed against the virus is very promising when applied early in the course of the disease, but its usefulness in advanced stages may be doubtful .
Similarly, the use of anti-inflammatory therapy applied too early may not be necessary and could even lead to viral replication, as in the case of corticosteroids.
There appear to be two distinct but overlapping pathological subsets :
- The first triggered by the virus.
- The second, the guest’s response.
Whether in the native state, in the immunoquiescent state as in the elderly, or in the immunosuppressed state as in heart transplantation, the disease tends to present and follow these two phases, although at different levels of severity.
Early reports on heart transplantation suggest that symptom expression during the establishment phase of infection is similar to that of non-immunosuppressed individuals; However, in limited series, the second wave determined by the host inflammatory response appears to be milder, possibly due to concomitant use of immunomodulatory drugs.
Similarly, an epidemiological study from Wuhan in a cohort of 87 patients suggests that precautionary measures of social distancing, disinfection, and general hygiene allow heart transplant recipients to experience a low rate of COVID-19 disease.
Of course, we do not know if they are asymptomatic carriers, since in this survey-based study, universal testing during the first 3 months was not employed. An interesting fact in this study was that many heart transplant recipients have hematologic changes of lymphopenia due to the effects of immunosuppressive therapy that may obfuscate laboratory interpretation of infection in such patients if they become infected.
| Much confusion abounds in the therapeutic tactics employed in COVID-19. It is imperative that a structured approach to clinical phenotyping be taken to distinguish the phase in which viral pathogenicity is dominant versus when the host inflammatory response overtakes the pathology. |
In this editorial, we propose a clinical staging system to establish a standardized nomenclature for uniform evaluation and reporting of this disease, to facilitate therapeutic application and evaluate response. We propose the use of a 3-stage classification system, recognizing that COVID-19 disease exhibits three degrees of increasing severity that correspond to distinct clinical findings, response to therapy, and clinical outcome (Figure).
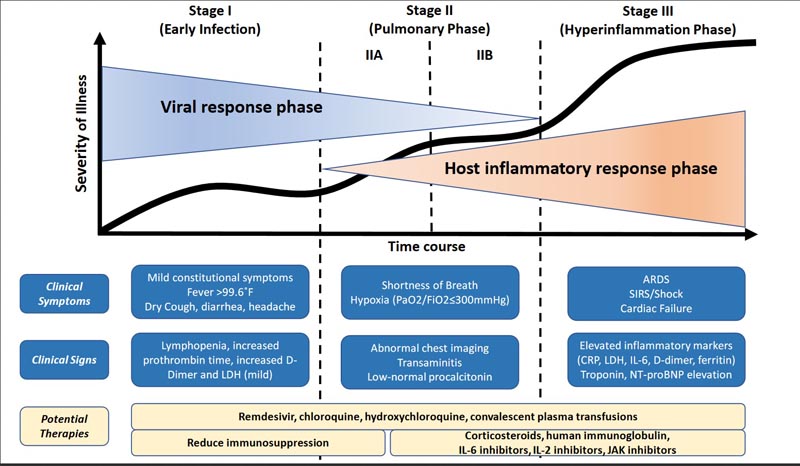
Figure 1: Classification of COVID-19 disease states and potential therapeutic targets Caption: The figure shows 3 increasing phases of disease progression with COVID-19, with associated signs, symptoms, and potential phase-specific therapies. ARDS = acute respiratory distress syndrome; CRP = C-reactive protein; IL = interleukin; JAK = Janus kinase; LDH = lactate dehydrogenase; SIRS = Systemic inflammatory response syndrome.
Stage I (mild), early infection:
The initial stage occurs at the time of inoculation and early establishment of the disease. For most people, this involves an incubation period associated with mild and often non-specific symptoms such as malaise, fever and dry cough. During this period, SARS-CoV-2 multiplies and takes up residence in the host, primarily focusing on the respiratory system .
Like its older relative, SARS-CoV (responsible for the 2002-2003 SARS outbreak), SARS-CoV-2 binds to its target using the angiotensin-converting enzyme 2 (ACE2) receptor on human cells. . These receptors are abundantly present in the epithelium of the human lung and small intestine, as well as in the vascular endothelium. As a result of the airborne method of transmission, as well as the affinity for lung ACE2 receptors, the infection usually presents with mild respiratory and systemic symptoms.
| Diagnosis at this stage includes respiratory sample PCR, serum testing for SARS-CoV-2 IgG and IgM, along with chest imaging, complete blood count (CBC), and liver function tests. The complete blood count may reveal lymphopenia and neutrophilia without other significant abnormalities. |
Treatment at this stage is aimed primarily at symptomatic relief. If a viable antiviral therapy (such as remdesivir) proves beneficial, targeting selected patients during this stage may reduce the duration of symptoms, minimize contagion, and prevent progression of severity.
In patients who can keep the virus limited to this stage of COVID-19, the prognosis and recovery are excellent.
Stage II (lung involvement (IIa) without hypoxia and (IIb) with hypoxia:
In the second stage of established lung disease, viral multiplication and localized inflammation in the lung is the norm.
- During this stage, patients develop viral pneumonia , with cough, fever, and possibly hypoxia (defined as a PaO2/FiO2 of <300 mmHg).
- Imaging with chest x-ray or computed tomography reveals bilateral infiltrates or ground-glass opacities .
- Blood tests reveal increased lymphopenia, along with transaminitis.
- Markers of systemic inflammation may be elevated, but not noticeably.
It is at this stage that most COVID-19 patients would need to be hospitalized for close observation and treatment.
Treatment would mainly consist of supportive measures and available antiviral therapies such as remdesivir ( available under compassionate use and trial). It should be noted that serum procalcitonin is low to normal in most cases of COVID-19 pneumonia.
In early stage II (without significant hypoxia), the use of corticosteroids can be avoided in patients with COVID-19.4
However, if hypoxia occurs , patients are likely to progress and require mechanical ventilation and in that situation, we believe that the use of anti-inflammatory therapy , such as with corticosteroids, may be helpful and can be employed judiciously.
Therefore, stage II disease should be subdivided into stage IIa (without hypoxia) and stage IIb (with hypoxia).
Stage III (severe) systemic hyperinflammation
A minority of patients with COVID-19 will progress to the third and most severe stage of the disease, which manifests as an extrapulmonary systemic hyperinflammation syndrome . At this stage, markers of systemic inflammation appear to be elevated. COVID-19 infection results in a decrease in helper, suppressor and regulatory T cell counts.
Studies have shown that inflammatory cytokines and biomarkers such as interleukin (IL)-2, IL-6, IL-7, granulocyte colony-stimulating factor, macrophage inflammatory protein 1-α, tumor necrosis factor- α, C-reactive protein, ferritin, and D-dimer are significantly elevated in those patients with more severe disease. Troponin and N-terminal pro B-type natriuretic peptide (NT-proBNP) may also be elevated.
A form similar to hemophagocytic lymphohistiocytosis (SHLH) may occur in patients at this advanced stage of the disease.
| At this stage, shock, vasoplegia, respiratory failure and even cardiopulmonary collapse can be detected. Systemic organ involvement, including myocarditis, would manifest during this stage. |
Personalized therapy in stage III depends on the use of immunomodulatory agents to reduce systemic inflammation before it overwhelmingly results in multi-organ dysfunction.
In this phase, the use of corticosteroids may be justified along with the use of cytokine inhibitors such as tocilizumab (IL-6 inhibitor) or anakinra (IL-1 receptor antagonist). Intravenous immunoglobulin (IVIG) may also play a role in modulating an immune system that is in a hyperinflammatory state. In general, the prognosis and recovery from this critical stage of the disease is poor, and rapid recognition and deployment of such therapy may have the greatest yield.
The first open-label randomized controlled clinical trial of antiviral therapy was recently reported . One reason for this may have been that patients were recruited during the hypoxic lung stage (stage IIb) when viral pathogenicity may have been only a minor dominant aspect of the overall pathophysiology, and host inflammatory responses were the predominant pathophysiology.
We believe that this proposed 3-stage classification system for COVID-19 disease will serve to develop a uniform scaffold to build a structured therapeutic experience as healthcare systems globally are besieged by this crisis, in patients with or without transplant.