Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease it causes, coronavirus disease 2019 (COVID-19), is an emerging health threat. As of February 2020, most cases were described in non-US health systems.
One of the first deaths in the United States was reported at Evergreen Hospital in Kirkland, Washington. Over the following weeks, multiple cases of COVID-19 were identified in the surrounding community and treated at Evergreen Hospital. Most were attributed to transmission in the US, and were related to exposures in a skilled nursing facility.
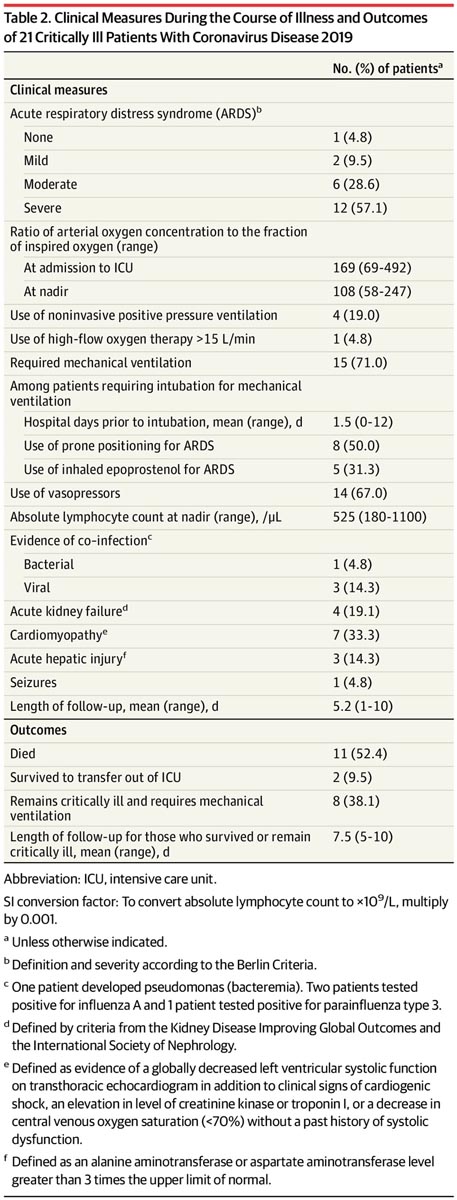
In this case series, we describe the clinical presentation, characteristics, and outcomes of incident COVID-19 cases admitted to the intensive care unit (ICU) at Evergreen Hospital to inform other physicians treating critically ill patients with COVID-19. 19.
Methods
Patients with confirmed SARS-CoV-2 infection (positive result by polymerase chain reaction test of a nasopharyngeal sample) admitted to the ICU at Evergreen Hospital between February 20, 2020 and March 5 were included. of 2020.
Evergreen Hospital is a 318-bed public hospital with a 20-bed ICU serving approximately 850,000 residents of King and Snohomish counties in Washington state.
Prior to data collection, an exemption was obtained from Evergreen Healthcare’s institutional review board. Data from deidentified patients were collected and analyzed using Stata version 15.1 (StataCorp).
- Laboratory tests were reviewed at ICU admission and on day 5.
- Chest radiographs were reviewed by an intensivist and a radiologist.
- Patient outcome data were assessed after 5 or more days of ICU care or at the time of death.
- A statistical significance analysis was not performed given the descriptive nature of the study.
Results
|
Discussion
This study represents the first description of critically ill patients infected with SARS-CoV-2 in the United States. These patients had a high rate of ARDS and a high risk of death, similar to data published in China. However, this case series adds information on early presentation and outcomes in this population and demonstrates poor short-term outcomes among patients requiring mechanical treatment. ventilation.
It is unclear whether the high rate of cardiomyopathy in this case series reflects a direct cardiac complication of SARS-CoV-2 infection or the result of overwhelming critical illness. Others have described cardiomyopathy in COVID-19, and additional research may better characterize this risk.
Limitations of this study include the small number of patients from a single center, the study population included older residents of skilled nursing facilities, and it is likely not widely applicable to other critically ill patients.
However, this study provides some initial experiences regarding the characteristics of COVID-19 in critically ill patients in the US and emphasizes the need to limit the exposure of nursing home residents to SARS-CoV-2. .