Research Highlights:
|
Summary
Background:
The risk of major adverse cardiovascular events increases substantially after stroke. Although exercise-based cardiac rehabilitation has been shown to improve prognosis after cardiac events, it is not part of routine care for people who have had a stroke. Therefore, we investigated the association between cardiac rehabilitation and major adverse cardiovascular events for people after stroke.
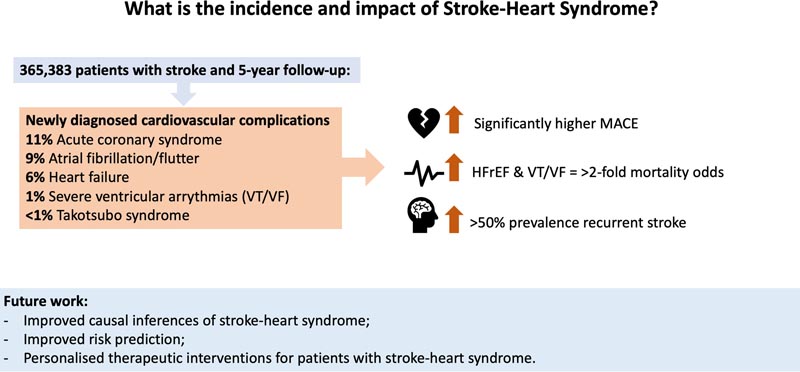
After a stroke, people are at increased risk of new-onset cardiovascular complications. However, the incidence and long-term clinical consequences of newly diagnosed cardiovascular complications after stroke are unclear.
The aim of the present study was to investigate the incidence and long-term clinical outcomes of newly diagnosed cardiovascular complications after incident ischemic stroke.
Methods:
A retrospective cohort study was conducted using de-identified electronic medical records from 53 participating healthcare organizations. Patients with incident ischemic stroke aged ≥18 years with 5 years of follow-up were included.
Patients who were diagnosed with new-onset cardiovascular complications (heart failure, severe ventricular arrhythmia, atrial fibrillation, ischemic heart disease, Takotsubo syndrome) within 4 weeks (exposure) of the incident ischemic stroke had a 1:1 propensity score (age, sex, ethnicity, comorbidities, cardiovascular care) with ischemic stroke patients who were not diagnosed with a new-onset cardiovascular complication (control).
Logistic regression models produced odds ratios (ORs) with 95% CIs for the 5-year incidence of all-cause mortality, recurrent stroke, hospitalization, and acute myocardial infarction.
Results:
Of 365,383 stroke patients with 5-year follow-up: 11.1% developed acute coronary syndrome; 8.8% atrial fibrillation/flutter; heart failure 6.4%; 1.2% serious ventricular arrhythmias; and 0.1% Takotsubo syndrome within 4 weeks of the incident ischemic stroke.
After propensity score matching, the odds of 5-year all-cause mortality were significantly higher in patients with stroke and acute coronary syndrome (odds ratio, 1.49 [95% CI, 1.44– 1.54]), atrial fibrillation/flutter (1.45 [1.40–1.50 ]), heart failure (1.83 [1.76–1.91]), and severe ventricular arrhythmias (2.08 [ 1.90–2.29]), compared to matched controls.
The odds of 5-year rehospitalization and acute myocardial infarction were also significantly higher for stroke patients diagnosed with new-onset cardiovascular complications.
Takotsubo syndrome was associated with significantly higher odds of 5-year composite major adverse cardiovascular events (1.89 [1.29–2.77]). Atrial fibrillation/flutter was the only new-onset cardiac complication associated with significantly higher odds of recurrent ischemic stroke at 5 years (1.10 [1.07-1.14]).
Conclusions:
- New-onset cardiovascular complications diagnosed after ischemic stroke are very common and are associated with a significantly worse 5-year prognosis in terms of major adverse cardiovascular events.
- Individuals with newly diagnosed stroke and cardiovascular complications had a >50% prevalence of recurrent stroke at 5 years.
Comments
People who survive an ischemic stroke are much more likely to develop major heart complications during the first month after the stroke and, as a result, also have a higher risk of death, heart attack or another stroke within five years, compared to people who do not develop heart problems soon after a stroke, according to new research published today in Stroke , the peer-reviewed flagship journal of the American Stroke Association , a division of the American Heart Association .
Ischemic stroke is the most common type of stroke, accounting for 87% of all strokes, and occurs when blood flow to the brain is blocked. After a stroke, people often have cardiovascular complications, known as stroke heart syndrome.
Cardiac complications include acute coronary syndrome, angina (chest pain), heart rhythm problems such as atrial fibrillation, arrhythmia, and ventricular fibrillation; heart attack; heart failure or Takotsubo syndrome (broken heart syndrome), a type of temporary, stress-induced enlargement of a part of the heart that affects its ability to pump effectively. These conditions increase the risk of disability or death in the short term, but the long-term consequences for people with stroke syndrome are unknown.
“We know that heart disease and stroke share similar risk factors, and there is a bidirectional relationship between the risk of stroke and heart disease. For example, heart conditions like atrial fibrillation increase the risk of stroke, and stroke also increases the risk of heart conditions,” said Benjamin JR Buckley, Ph.D., lead author of the study and postdoctoral researcher in preventive cardiology. at the Liverpool Center for Cardiovascular Science, University of Liverpool in the United Kingdom. "We wanted to know how common newly diagnosed cardiac complications are after a stroke and, more importantly, whether heart-stroke syndrome is associated with an increased risk of long-term major adverse events."
Researchers analyzed the medical records of more than 365,000 adults treated for ischemic stroke at more than 50 health care facilities, primarily in the United States, between 2002 and 2021. People diagnosed with stroke and complications Heart complications within four weeks after the stroke were compared with an equal number of stroke survivors who did not have these heart complications within four weeks (the control group).
After adjusting for potential confounders, such as age, sex, and race/ethnicity, and comparing stroke survivors who had new heart complications with those who did not, the analysis found:
- Overall, among all stroke survivors in the study, approximately 1 in 10 (11.1%) developed acute coronary syndrome, 8.8% were diagnosed with atrial fibrillation, 6.4% developed heart failure, 1, 2% exhibited severe ventricular arrhythmias and 0.1% developed “broken heart” within four weeks of the stroke.
- The risk of death within five years after a stroke increased significantly among participants with new cardiac complications: 49% more likely if they had developed acute coronary syndrome; 45% more likely if they had developed atrial fibrillation/flutter; and 83% more likely if they developed heart failure. Severe ventricular arrhythmias doubled the risk of death.
- The likelihood of hospitalization and heart attack within five years of a stroke was also significantly higher among those who developed heart complications within the one-month window.
- Stroke survivors with Takotsubo syndrome were 89% more likely to suffer a major cardiac event within five years of their stroke.
- People who developed atrial fibrillation after a stroke were 10% more likely to have a second stroke within five years of the stroke.
- People with newly diagnosed stroke and cardiovascular complications were 50% more likely to have a recurrent stroke within five years of their first stroke.
"I was especially surprised by how common stroke syndrome was and the high rate of recurrent stroke across all subgroups of adults with stroke syndrome," Buckley said. “This means that this is a high-risk population that we need to focus more secondary prevention efforts on.”
The study results build on the understanding of the bidirectional link between the brain and the heart and extend this understanding to long-term health outcomes. “We are working on additional research to determine how stroke heart syndrome can be best predicted,” Buckley said.
“We also need to develop and implement treatments to improve outcomes for people with stroke syndrome,” Buckley said. “For example, comprehensive exercise-based rehabilitation may be helpful after a stroke, so for people with stroke and newly developed cardiac complications, it should also be beneficial, perhaps even more so. “I think this is an interesting area for future research.”
Limitations of the study include that this is a retrospective analysis and it is unclear whether cardiac complications diagnosed after ischemic stroke were caused by stroke or contributed to stroke.
“This research underscores why it is so important for neurologists and cardiologists to work hand-in-hand with their patients and each other to understand why the first stroke occurred and perform a comprehensive evaluation to identify new risk factors for another stroke and cardiovascular disease that may require initiation of preventive therapies,” said Lee H. Schwamm, MD, volunteer chair of the American Stroke Association Advisory Committee and C. Miller Fisher Chair of Vascular Neurology at Massachusetts General Hospital in Boston. . “The American Stroke Association recommends a personalized secondary stroke prevention plan for all stroke survivors.”
















