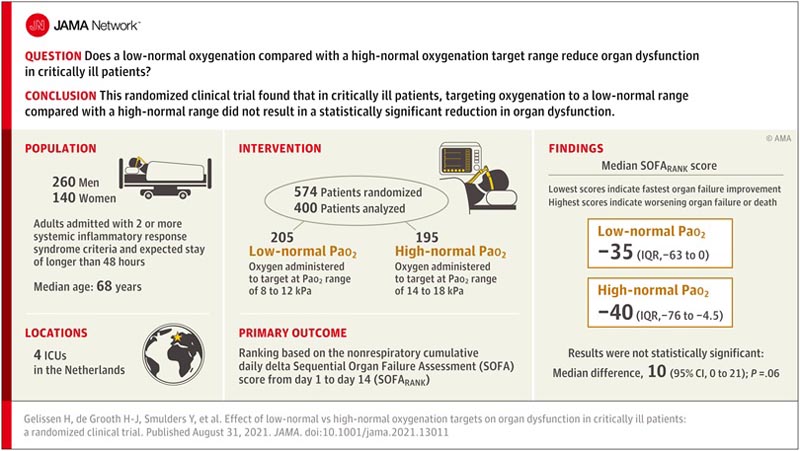
Key points Does low normal oxygenation compared to a target range of high normal oxygenation reduce organ dysfunction in critically ill patients? Findings This randomized clinical trial included 400 patients in the intensive care unit with at least 2 positive systemic inflammatory response syndrome criteria . Randomization to a target Pao2 range of 8 to 12 kPa versus 14 to 18 kPa resulted in a median SOFARANK score of -35 versus -40 (a lower score represents less severity of organ failure), a difference that was not statistically significant. Meaning Among critically ill patients, directing oxygenation to a low normal range compared to a high normal range did not result in a statistically significant reduction in organ dysfunction. |
Oxygen is often given liberally in the intensive care unit (ICU) to treat or prevent hypoxemia. For many years, oxygen was considered to have consistently favorable effects. However, an observational study using data from 1999 to 2006 showed a U-shaped relationship between Pao2 and mortality which opened a debate about optimal oxygenation goals in critically ill patients.
Potential negative effects of hyperoxemia include pulmonary toxicity, increased ischemia/reperfusion injury, and systemic vasoconstriction with decreased organ perfusion3. These effects may affect more than improve oxygen delivery to tissues.4
On the contrary, hyperoxemia can also have benefits. Systemic vasoconstriction can reduce vasodilation in patients with systemic inflammatory response syndrome5 (SIRS) and favorably redistribute blood flow to organs. Hyperoxemia can also have antimicrobial effects6.
Six randomized clinical trials (RCTs) in ICU patients7 and one meta-analysis comparing low versus high oxygenation goals showed inconsistent results. Two of these trials8 and the meta-analysis reported a reduction in mortality for lower oxygenation targets, while 4 trials showed no difference in outcomes. One trial reported a higher incidence of mesenteric ischemia in the low oxygenation target group.
The aim of this trial was to investigate whether a low normal Pao2 target compared to a high normal Pao2 target (avoiding toxic Fio2 values) in critically ill patients with systemic inflammation leads to better organ function.
Importance
Hyperoxemia may increase organ dysfunction in critically ill patients, but optimal oxygenation targets are unknown.
Aim
To determine whether a low normal Pao2 target compared to a high normal target reduces organ dysfunction in critically ill patients with systemic inflammatory response syndrome (SIRS).
Design, environment and participants
Multicenter randomized clinical trial in 4 intensive care units in the Netherlands. Enrollment was from February 2015 to October 2018, with follow-up ending in January 2019, and included adult patients admitted with 2 or more SIRS criteria and an expected length of stay of more than 48 hours. A total of 9925 patients were assessed for eligibility, of whom 574 met enrollment criteria and were randomized.
Interventions
Target Pao2 ranges were 8 to 12 kPa (low normal, n = 205) and 14 to 18 kPa (high normal, n = 195). A fraction of inspired oxygen greater than 0.60 was applied only when clinically indicated.
Main results and measures
The primary endpoint was SOFARANK, a graded outcome of nonrespiratory organ failure quantified by the nonrespiratory components of the Sequential Organ Failure Assessment (SOFA) score, summed over the first 14 days of the study.
Participants were ranked from the most rapid improvement in organ failure (lowest scores) to worsening of organ failure or death (highest scores).
Secondary endpoints were duration of mechanical ventilation, in-hospital mortality, and hypoxemic measurements.
Results
Among the 574 patients who were randomized, 400 (70%) were enrolled within 24 hours (median age, 68 years; 140 women [35%]), all of whom completed the trial. The median difference in Pao2 between groups was -1.93 kPa (95% CI, -2.12 to -1.74; P < 0.001).
The median SOFARANK score was -35 points in the low-normal Pao2 group versus -40 in the high-normal Pao2 group (median difference, 10 [95% CI, 0 to 21]; P = 0 ,06).
There was no significant difference in the mean duration of mechanical ventilation (3.4 vs. 3.1 days; median difference, −0.15 [95% CI, −0.88 to 0.47]; P = 0.59) and in-hospital mortality (32% vs. 31%; odds ratio, 1.04 [95% CI, 0.67 to 1.63]; P = 0.91).
Mild hypoxemic measurements occurred more frequently in the low-normal group (1.9% vs. 1.2%; median difference, 0.73 [95% CI, 0.30 to 1.20]; p <0.001).
Acute renal failure developed in 20 patients (10%) in the low-normal Pao2 group and 21 patients (11%) in the high-normal Pao2 group, and acute myocardial infarction in 6 patients (2.9%) in the normal-low Pao2 group. group and 7 patients (3.6%) in the high normal Pao2 group.
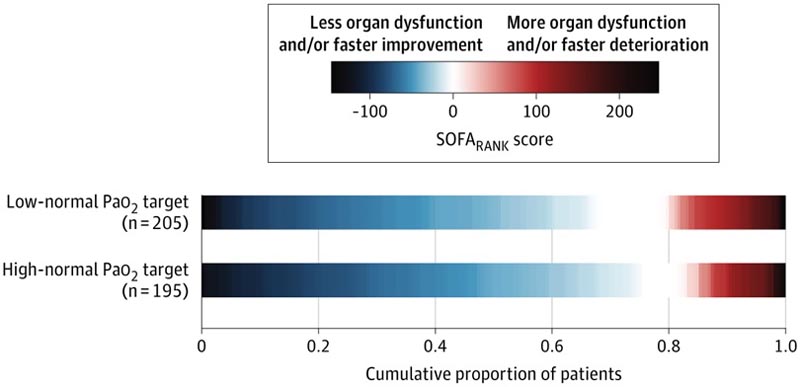
The primary endpoint was a graded outcome of nonrespiratory organ failure quantified by the nonrespiratory components of the Sequential Organ Failure Assessment (SOFA) score. For each patient, the daily SOFA score minus the baseline SOFA score was summed over the first 14 days of the study. The resulting score was used to classify participants from the most rapid improvement in organ failure (lower scores) to worsening organ failure or death (higher scores). The figure shows that patients randomized to a high normal Pao2 target had non-significantly lower (better) scores. The median SOFARANK score was −35 points (interquartile range [IQR], −63 to 0) in the low-normal group versus −40 points (IQR, −76 to −4.5) in the normal group high (median difference, 10 points [95% CI, 0 to 21]; p = 0.06).
Discussion
In this multicenter RCT that included 400 critically ill patients with 2 or more SIRS criteria, treatment with a low normal Pao2 target (8-12 kPa) compared with a high normal target (14-18 kPa) did not significantly reduce organic dysfunction in 14 days.
There were no significant differences in 90-day mortality, duration of mechanical ventilation, or length of ICU stay.
The high-normal Pao2 targets were based on current clinical practice and avoidance of the potential detrimental effects of severe hyperoxemia. The Fio2 to achieve the high normal target was restricted to a maximum of 0.60. In comparison, previous trials did not report an upper limit of Fio2 to achieve the goal of high oxygenation.
The present trial investigating critically ill patients with signs of systemic inflammation showed better resolution of non-respiratory organ failure in the high normal group compared to the low normal group, but this difference was not statistically significant.
There was a small but significant increase in the incidence of hypoxemia in the low-normal Pao2 target group, but a much larger increase in the incidence of hyperoxemia in the high-normal Pao2 target group.
Overall, the balance of the effects of hypoxemia versus hyperoxemia remains unclear. The body of trials investigating mild hyperoxemic versus normoxemic targets, including the current study, have not clearly demonstrated an effect on outcomes. The effect of hyperoxemia is likely to be smaller than has been hypothesized (the aim of the Mega-ROX trial currently underway [UMIN Clinical Trials Registry UMIN000042551]) is to detect a possibly very small effect or an effect only present at values more extremes of hyperoxemia.
Conclusions and relevance Among critically ill patients with 2 or more SIRS criteria, treatment with a low-normal Pao2 target compared with a high-normal Pao2 target did not result in a statistically significant reduction in organ dysfunction. However, the study may have had limited power to detect a smaller treatment effect than had been hypothesized. |















