The researchers used data from nearly 150,000 adults who visited the emergency department or were admitted with COVID-19 from March to December 2020. About 28% of this group were overweight (BMI, 25-29.9) and 51% was obese (BMI, 30+).
After multivariable adjustment, being overweight was associated with an increased risk of invasive mechanical ventilation (hazard ratio, 1.12) compared with being at a healthy weight.
Being obese was associated with increased risks of hospitalization, ICU admission (BMI, 40 or more only), invasive mechanical ventilation, and death, with the risk increasing with higher BMI. The risks associated with higher weight were greater for adults younger than 65 years than for older adults.
The authors write: "The finding that the risk of severe disease associated with COVID-19 increases with higher BMI suggests that progressively intensive management of COVID-19 may be necessary for patients with more severe obesity. This finding also supports the "We hypothesize that inflammation due to excess adiposity could be a factor in the severity of the disease associated with COVID-19."
Summary What is already known about this topic? Obesity increases the risk of severe disease associated with COVID-19. What does this report add? Among 148,494 US adults with COVID-19, a non-linear relationship was found between body mass index (BMI) and COVID-19 severity, with lower risks in BMI near the threshold between healthy weight and overweight in the majority of cases, and then increases with higher BMI. Overweight and obesity were risk factors for invasive mechanical ventilation. Obesity was a risk factor for hospitalization and death, especially among adults younger than 65 years. What are the implications for public health practice? These findings highlight the clinical and public health implications of higher BMI, including the need for intensive disease management associated with COVID-19, continued vaccine prioritization and masking, and policies to support healthy behaviors. |
Obesity is a recognized risk factor for severe COVID-19, possibly related to chronic inflammation that disrupts immune and thrombogenic responses to pathogens, as well as impaired lung function from excess weight .
Obesity is a common metabolic disease that affects 42.4% of American adults (5) and is a risk factor for other chronic diseases, such as type 2 diabetes, heart disease, and some cancers.
The Advisory Committee on Immunization Practices considers obesity a high-risk medical condition for COVID-19 vaccine prioritization. Using data from the Premier Healthcare Database Special COVID-19 Release (PHD-SR),
CDC evaluated the association between body mass index (BMI) and the risk of severe COVID-19 outcomes (i.e., hospitalization, intensive care unit [ICU] or step-down unit admission, invasive mechanical ventilation, and death) .
Among 148,494 adults who were diagnosed with COVID-19 during an emergency department (ED) visit or as an inpatient at 238 US hospitals between March and December 2020, 28.3% were overweight and 50 .8% were obese.
- Overweight and obesity were risk factors for invasive mechanical ventilation and obesity was a risk factor for hospitalization and death, particularly among adults younger than 65 years.
- The risks of hospitalization, ICU admission, and death were lowest among patients with BMIs of 24.2 kg/m2, 25.9 kg/m2, and 23.7 kg/m2, respectively, and then increased dramatically with higher BMIs. high.
- The risk of invasive mechanical ventilation increased across the entire BMI range, from 15 kg/m2 to 60 kg/m2.
As physicians develop care plans for patients with COVID-19, they should consider the risk of serious outcomes in patients with higher BMIs, especially for those with severe obesity.
These findings highlight the clinical and public health implications of higher BMI, including the need for intensive management of COVID-19 disease as obesity severity increases, promotion of COVID-19 prevention strategies that include continued prioritization of vaccines and the use of face masks and policies to ensure community access to nutrition and physical activities that promote and support a healthy BMI.
Among 3,242,649 patients ≥18 years of age with documented height and weight who received emergency or inpatient care in 2020, a total of 148,494 (4.6%) had ICD-10-CM codes indicating a diagnosis of COVID-19.
Among 71,491 patients hospitalized with COVID-19 (48.1% of all COVID-19 patients), 34,896 (48.8%) required ICU admission, 9,525 (13.3%) required invasive mechanical ventilation, and 8,348 (11 .7%) died.
Approximately 1.8% of patients were underweight , 28.3% were overweight , and 50.8% were obese .
Compared with the total PHD-SR cohort, patients with COVID-19-associated disease were older (median age 55 years vs. 49 years) and had a higher crude prevalence of obesity (50.8% vs. 43.1%).
Obesity was a risk factor for both hospitalization and death, and showed a dose-response relationship with increasing BMI category: aRRs for hospitalization ranged from 1.07 (95% confidence interval [ CI = 1.05 to 1.09]) for patients with a BMI of 30 to 34.9 kg/m2 to 1.33 (95% CI = 1.30–1.37) for patients with a BMI ≥ 45 kg/m2 compared to those with a BMI of 18.5–24.9 kg/m2 (healthy weight).
The aRRs for death ranged from 1.08 (95% CI = 1.02-1.14) for those with a BMI of 30-34.9 kg/m2 to 1.61 (95% CI = 1.47-1.76) for those with a BMI ≥45 kg / m2.
Severe obesity was associated with ICU admission, with aRR of 1.06 (95% CI = 1.03-1.10) for patients with a BMI of 40-44.9 kg/m2 and 1.16 (95% CI = 1.11-1.20) for those with a BMI ≥ 45 kg/m2.
Overweight and obesity were risk factors for invasive mechanical ventilation , with aRR of 1.12 (95% CI = 1.05-1.19) for a BMI of 25-29.9 kg/m2 a 2, 08 (95% CI = 1.89-2.29) for a BMI ≥ 45 kg/m2.
Associations with risk of hospitalization and death were pronounced among adults younger than 65 years: aRRs for patients in the highest BMI category (≥45 kg/m2) compared with healthy weight patients were 1. 59 (95% CI = 1.52-1.67) for hospitalization and 2.01 (95% CI = 1.72-2.35) for death.
COVID-19 patients with low weight had a 20% (95% CI = 16%-25%) higher risk of hospitalization than those with a healthy weight.
Patients <65 years of age with low weight were 41% (95% CI = 31%-52%) more likely to be hospitalized than those with a healthy weight, and patients ≥65 years of age with low weight were 7% more likely to be hospitalized. (95% CI = 4%-10%) more likely to be hospitalized.
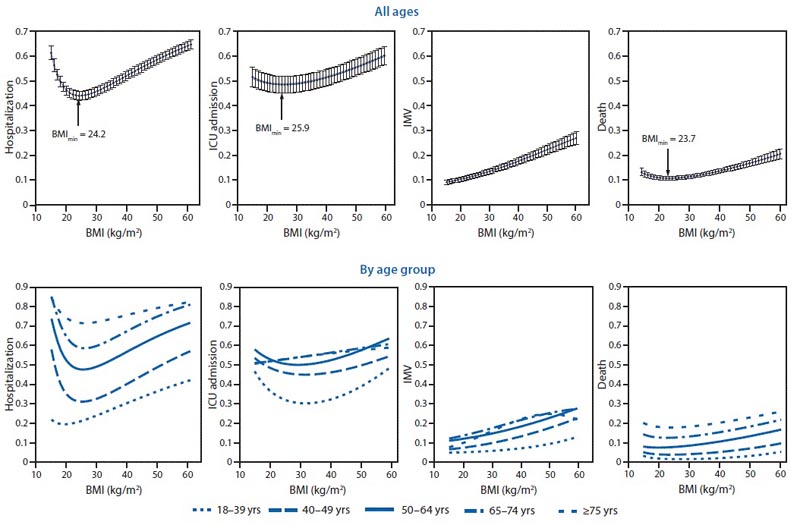
Estimated risk of severe illness associated with COVID-19* among adults aged 18 years and older, by body mass index (BMI) and age group - Premier Healthcare Special COVID-19 Release (PHD-SR), United States, March to December, 2020. Abbreviations : ICU = intensive care unit. IMV = invasive mechanical ventilation.
Discussion
Half (50.8%) of adult COVID-19 patients in this analysis were obese, compared to 43.1% in the total PHD-SR sample and 42.4% nationally (5) , suggesting that adults with COVID-19-associated disease and obesity may typically receive intensive care in emergency departments or hospitals.
The findings of this report are similar to those of previous studies indicating an increased risk of severe disease associated with COVID-19 among people with excess weight and provide additional information on a dose-response relationship between higher BMI and the risk of hospitalization, ICU admission. , invasive mechanical ventilation and death.
The finding that the risk of severe disease associated with COVID-19 increases with higher BMI suggests that progressively intensive management of COVID-19 may be necessary for patients with more severe obesity.
This finding also supports the hypothesis that inflammation due to excess adiposity could be a factor in the severity of the disease associated with COVID-19 (3,8). The positive association found between low weight and the risk of hospitalization could be explained by undetected underlying medical conditions or by deficiencies in the availability of essential nutrients and the immune response.
Consistent with previous studies, the dose-response relationship between the risk of hospitalization or death and higher BMI was particularly pronounced among patients <65 years of age (1,2). However, unlike previous studies that demonstrated little or no association between obesity and COVID-19 severity in older patients, the results of this report indicate that overweight and obesity are risk factors for invasive mechanical ventilation and that obesity or severe obesity are risk factors for hospitalization, ICU admission and death in patients ≥65 years of age.
A sensitivity analysis adjusting for other underlying medical conditions found weaker associations between BMI and COVID-19-associated severe illness, which could be partially attributable to indirect effects of obesity on COVID-19 or over-adjustment to include intermediate variables in the causal pathway from exposure (i.e., BMI) to outcome.
BMI is continuous in nature, and the analyzes in this report describe a J-shaped association between BMI and severe COVID-19, with the lowest risk in BMI near the threshold between healthy weight and overweight in most cases.
The risk of invasive mechanical ventilation increased across the BMI range, possibly due to impaired lung function associated with higher BMI).
These results highlight the need to promote and support a healthy BMI, which could be especially important for populations disproportionately affected by obesity, particularly Hispanic or Latino adults and non-Hispanic blacks and people from low-income households. which are populations that have a higher rate of obesity. prevalence of obesity and are more likely to have worse COVID-19 outcomes compared to other populations.
The findings of this study are subject to at least five limitations .
- First, risk estimates for severe illness associated with COVID-19 (including hospitalization) were measured only among adults who received care in a hospital; therefore, these estimates may differ from the risk among all adults with COVID-19.
- Second, hospitalization risk estimates could have been affected by bias introduced by hospital admission factors other than COVID-19 severity, such as a healthcare professional’s anticipation of future severity.
- Third, only patients with reported weight and height information were included; Among 238 hospitals, 28% of patients were missing information on height, weight, or both. However, the results of a sensitivity analysis using multiple imputation of missing BMIs were consistent with the primary findings.
- Fourth, the BMI of some older adults may have been misclassified due to complex interactions between height loss and sarcopenia, a condition characterized by loss of skeletal muscle mass and function.
- Finally, although this analysis includes one of the largest samples of patients with heights and weights available for evaluation to date, the results are not representative of the entire US patient population.
The findings of this report highlight a dose-response relationship between higher BMI and severe COVID-19-associated disease and underscore the need for progressively intensive disease management as the severity of obesity increases.
Continued strategies are needed to ensure community access to nutrition and physical activity opportunities that promote and support a healthy BMI. Prevention of COVID-19 in adults with higher BMIs and their close contacts remains important and includes multifaceted protective measures such as masking, as well as continued vaccine prioritization (6) and outreach for this population.