Summary Achalasia is a rare esophageal mobility disorder characterized by dysphagia. Patients often also suffer from chest pain, regurgitation and weight loss. Barium esophagography shows esophageal dilation with narrowing of the gastroesophageal junction. Manometry shows alteration or absence of peristalsis, as well as alteration of relaxation of the lower esophageal sphincter (LES). High-resolution manometry makes a more precise diagnosis of achalasia, its subtypes, and differentiation from other esophageal motor disorders. Possible treatments include some drugs, endoscopic botulinum toxin injection, balloon dilation, surgery (laparoscopic Heller myotomy), and a new, less invasive Heller myotomy procedure with transluminal surgery through the natural orifices. (NOTES) called peroral endoscopic myotomy (POEM). This intervention is comparable to traditional surgery in terms of its clinical success and its radiological and manometric results. |
► INTRODUCTION
Achalasia is an esophageal mobility disorder characterized by absence of esophageal peristalsis and deficiency in relaxation of the lower esophageal sphincter (LES). These anomalies are produced by alteration of the inhibitory innervation of the esophageal smooth muscle and the LES.1 Achalasia can be autoimmune, secondary to viral infection or neurodegenerative.1
Secondary achalasia or “pseudoachalasia” is secondary to a malignant tumor or other entities, such as Chagas disease or bariatric surgery. Achalasia is diagnosed by the combination of esophagography and esophageal manometry. The disease can be treated effectively in most patients by pneumatic dilation, Heller esophagomyotomy, and, more recently, peroral endoscopic myotomy (POEM).2
► EPIDEMIOLOGY
The epidemiology of achalasia has not been well studied. The prevalence in Europe is around 10 cases per 100,000 inhabitants, with an incidence of one new case per 100,000 inhabitants per year.3 The highest incidence is between 30 and 60 years of age and there are no differences according to sex.
Although the incidence is low, the chronic nature of achalasia affects health-related quality of life, work productivity, and functional status 4 According to longitudinal demographic studies, the disease does not significantly affect life expectancy.1
► PATHOPHYSIOLOGY
In achalasia, the inhibitory innervation of the esophageal smooth muscle and the LES is affected.5-8 An inflammatory process produces degeneration of the ganglion cells of the myenteric plexus of the esophageal body and the LES, thus losing the inhibitory neurotransmitters nitric oxide and vasoactive intestinal polypeptide. . The inflammatory reaction is associated with T cell infiltration, which leads to the slow destruction of ganglion cells.8
The underlying cause is unknown, but may be autoimmune, secondary to viral infection, or neurodegenerative. It can also be a manifestation of Chagas disease, caused by infection with Trypanosoma cruzi and characterized by generalized destruction of the myenteric plexus.9 There is a genetic predisposition when achalasia is associated with syndromes such as Aligrove or Down syndrome.10 eleven
► CLINICAL PICTURE
Suspect achalasia in patients with dysphagia on solids and liquids with regurgitation that does not respond to proton pump inhibitors.
Idiopathic achalasia can occur at any age, from childhood to old age. Its course is slow and when the patient consults the symptoms have been present for several years.1
Dysphagia is the main symptom of achalasia, present in 98% of cases12; It is with both solids and liquids and slowly worsens over time until it becomes a constant problem.
Dysphagia and sitophobia (fear of eating) can lead to weight loss, present in more than half of patients.12
Regurgitation of undigested food that accumulates in the dilated esophagus is observed in 78% of patients.1 It occurs more frequently at night because in the recumbent position there is no effect of gravity. Regurgitation can lead to aspiration manifesting as nocturnal cough, aspiration pneumonia, and even lung abscess.
Chest pain may occur (about 42% of patients), but is rarely severe.5-12 Burning discomfort in the epigastric area may be secondary to stasis esophagitis, drug-induced ulcers, or candidal esophagitis.6 In Untreated achalasia, regurgitation and dysphagia can lead to the diagnosis of gastroesophageal reflux disease (GERD) and the indication of proton pump inhibitors (PPIs).5 13 In general, true heartburn is not observed in untreated achalasia, 5 but it can be observed after treatment with pneumatic dilation, Heller esophagomyotomy or POEM.5
► ASSOCIATED ALTERATIONS
Distal esophageal acid exposure has been documented in 2-20% of patients with untreated achalasia.13 14 In untreated patients, 24-hour pH tracings may show episodes of reflux or prolonged episodes of acid exposure with difficulty swallowing. remove acid 15 16
Patients with achalasia may suffer inflammatory changes of the distal esophagus through three mechanisms: infection, stasis, and caustic injury.1
Epiphrenic diverticula are believed to represent pulsion diverticula, caused by increased intraluminal esophageal pressure. They are not specific to achalasia. Two-thirds of patients with epiphrenic diverticula have manometric disorders, such as diffuse esophageal spasm or achalasia.5
Patients with long-standing achalasia may progress to a markedly dilated esophagus (megaesophagus). Myotomy can be performed, but esophagectomy (open, thoracoscopic, minimally invasive) and interposition of the colon, stomach, or jejunum may be the best option.17
► CANCER
Patients with long-standing achalasia are at increased risk of developing squamous esophageal carcinoma (3.5% of patients).2 The average time from the onset of achalasia symptoms to cancer detection is 25 years.19-21 It has been suggested that this occurs primarily in untreated achalasia and is caused by chronic esophageal stasis and inflammation.19 Massive esophageal dilation, long-standing achalasia, and smoking are predisposing factors.23
A study of 331 patients undergoing pneumatic dilation observed 28 new cases of Barrett’s esophagus and two new cases of Barrett’s adenocarcinoma during a mean follow-up of 8.9 years.24
Gastroenterologists often perform periodic surveillance, although there are no data to support routine endoscopy, which is at the physician’s discretion. The American Society of Gastrointestinal Endoscopy (ASGE) does not mandate cancer surveillance in achalasia, but considers monitoring 15 years after the initial diagnosis “reasonable.”
► IMITATIONS AND DIFFERENTIAL DIAGNOSIS; SECONDARY ACHALASIA
Secondary achalasia is the appearance of clinical, radiographic and manometric data of achalasia caused by an underlying disease. Secondary achalasia can occur with cancer, Chagas disease and intestinal pseudo-obstruction, as well as after surgery. Achalasia secondary to malignant tumors, also called pseudoachalasia , is responsible for only 4% of patients with manometric data of achalasia1, with 75% of cases being adenocarcinoma of the cardia.26
This syndrome can also be caused by non-contiguous forms of cancer, including lymphoma and malignant tumors of the lung, pancreas, prostate and liver. Three characteristics are suggestive of cancer as a cause of achalasia: duration of dysphagia <1 year, significant weight loss (>6.8 kg), and age >55 years.22-27
The diagnosis may not be evident on esophagography and endoscopy, and thoracoabdominal computed tomography and endoscopic ultrasound may be necessary. Peristalsis may also be absent in the middle and distal esophagus in scleroderma, but is preserved in the striated muscle of the upper third of the esophagus and LES smooth muscle pressure is usually low.7
Achalasia may occur after surgery.28 Severe dysphagia occurs after surgical vagotomy in some patients.29 An achalasia-like syndrome may also occur after a too-tight fundoplication at the gastroesophageal junction (GEJ).30
► DIAGNOSIS
Diagnostic evaluation in patients with dysphagia usually begins with esophagography to rule out an anatomical lesion of the esophagus, such as stricture or cancer. Achalasia can be detected in most patients through radiology,27 where the esophagus is seen dilated and occasionally with excess secretions and food.32.
• Esophageal manometry
It is the reference method for the diagnosis of achalasia. The two classic manometric findings in the diagnosis of achalasia are aperistalsis of the esophageal body and insufficient relaxation of the LES during swallowing. Peristaltic contractions are not usually observed in the esophageal body.5-32 Esophageal contractions are usually low amplitude and simultaneous throughout the entire esophagus.32 In patients with achalasia, relaxation of the LES is absent or incomplete.5 -32 Residual pressure between the esophagus and stomach produces functional obstruction, which in turn leads to esophageal dilation and stasis. Baseline LES pressure is increased in about two-thirds of patients.32
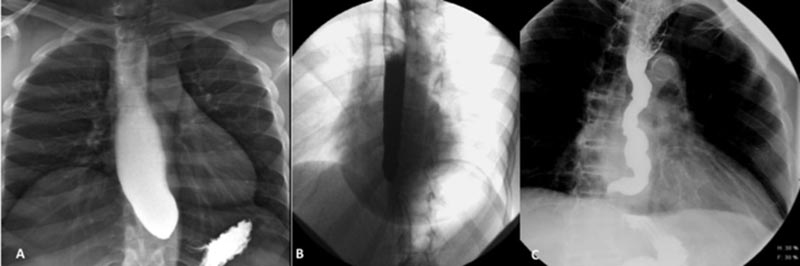
• Radioscopy
In early achalasia, fluoroscopy can detect the breakdown of normal peristaltic esophageal contraction into numerous simultaneous tertiary contractions of the esophageal body and the failure of the primary wave to clear the esophagus. Classically, peristalsis is absent throughout the esophageal body.32 The distal esophagus is generally reduced to a characteristic “bird-beak” narrowing. This represents the upper edge of the LES that cannot relax normally. The esophagus is not completely emptied of the introduced barium. These data should prompt endoscopy and manometry to be performed.
• Videoesophagography
Studies suggest that video esophagography has good sensitivity (58%-95%) in relation to esophageal manometry to detect esophageal dilation, narrowing of the EGJ, and lack of peristalsis. 33-35 The American Gastrointestinal Association (AGA) recommendations strongly advise endoscopic evaluation of the GEJ and cardia in all patients with achalasia. Radiological examination also objectively evaluates esophageal emptying. The timed barium esophagram helps to evaluate the severity of achalasia and also to estimate the success of treatment.36 37-39
• Endoscopy
Endoscopy is used in patients with achalasia to rule out other diseases and to diagnose complications. In idiopathic achalasia, the mucosa is normal and there is mild to moderate resistance to passage of the endoscope through the EGJ. Intense resistance may suggest an infiltrating tumor in or around the EGJ.40 Saliva, fluid, and undigested food particles may be observed in the esophagus and, in the absence of mucosal stricture or tumor, suggest achalasia.2 As the disease progresses, the dilation and tortuosity of the lumen make the diagnosis more obvious.
• High resolution esophageal manometry
High-resolution esophageal manometry (HRM) is a relatively recent advance.41 It detects esophageal shortening, presumably due to longitudinal muscle contractures. This shortening can produce movement in a cephalic direction of the high pressure zone (LES), which appears as an appropriate relaxation of the LES in common manometry, but not in MAR.39 41 The sensitivity of this method is 97%.35
Furthermore, with MAR, the LES shows a pattern of obstruction to EGJ flow with an increase in integrated residual pressure > 15 mm Hg in patients with achalasia and this provides a more objective measurement than the LES relaxation pressure used in traditional manometry.41 This integrated residual pressure figure was chosen to maximize sensitivity and specificity for detecting achalasia.
MAR also allows achalasia to be subclassified based on the contractility characteristics of the esophageal body. Three types of achalasia were defined based on the patterns of non-peristaltic esophageal pressurization that accompanies the increase in integrated residual pressure.42, 43
- Type I, with insufficient contractions and absence of esophageal pressurization with swallowing.
- Type II, with pan-esophageal pressurization with swallowing
- Type III, with spastic or premature contractions
Several studies show that type II achalasia, which is the most common, seems to have the most favorable therapeutic response, and type III, the least favorable. 2-43
According to the AGA recommendations, “esophageal mobility testing, esophagogastroduodenoscopy (EGD), and barium esophagram have complementary diagnostic functions.” EGD is essential to rule out pseudoachalasia; the other two studies have confirmatory functions.
► TREATMENT
The most effective treatments are pneumatic balloon dilation and surgical myotomy.
Treatment with smooth muscle relaxants is ineffective in achalasia. Other longer lasting therapeutic options are weakening or ablation of the LES, which can be endoscopic (botulinum toxin, pneumatic balloon dilation), surgical (laparoscopic, thoracoscopic, open abdominal myotomy) and more recently transluminal endoscopic surgery through natural orifices (NOTES) and the POEM. The most effective treatments are pneumatic balloon dilation and surgical myotomy. Its effectiveness is comparable in randomized controlled studies with follow-up of up to five years. POEM is performed endoscopically and therefore represents a refinement of surgical myotomy.
• Pharmacotherapy
Pharmacological treatment for achalasia is mainly with nitrates and calcium channel blockers. These medications reduce LES pressure and relieve dysphagia, with little or no effect on LES relaxation or esophageal peristalsis.5-45 Both the sublingual and oral forms have prohibitive side effects, including headache and dizziness.44 Calcium channel blockers have maximum effect 20-45 minutes after taking, with duration of effect of 30 - 120 minutes. The maximum effect of nitrates is three to 27 minutes after taking them, with a duration of effect of 30 - 90 minutes.
An observational study reported that the majority of patients treated with nifedipine had symptom improvement that persisted at one-year follow-up. 45 Other drugs, such as loperamide, cimetropium, and sildenafil, decrease LES pressure but do not relieve dysphagia in patients with achalasia.46-48
• Endoscopic botulinum toxin injection (ITBE)
Botulinum toxin (botox) is a potent inhibitor of acetylcholine release and its injection into the LES should mitigate cholinergic stimulation and lower LES pressure. In an initial validation series, 31 achalasia patients received Botox injections. ITBE achieved efficacy (decrease in Eckardt score to 3 or less) in 70% of patients at 18 months, although 40% required more than one injection.49 The medical literature is not uniform regarding dosage (25-100 U), technique and programming.
A prospective randomized study of 118 patients who received one of three doses (50, 100, 200 units) and one of two botox schedules (one injection or reinjection in 30 days), indicated that 68% of patients who received two doses of 100 U each one month apart still had a response after two years.50 A meta-analysis of nine prospective case-control and cohort studies indicated a 79% response at one month with a decrease in the same after three, six and 12 months (70%, 53%, 41%, respectively).51 Older patients and those with vigorous achalasia had a better response to treatment.52 The ease of administration of ITBE and the infrequent and usually mild adverse effects make This treatment may be attractive, but the limited duration of its effectiveness relegates it to use in frail and elderly patients.
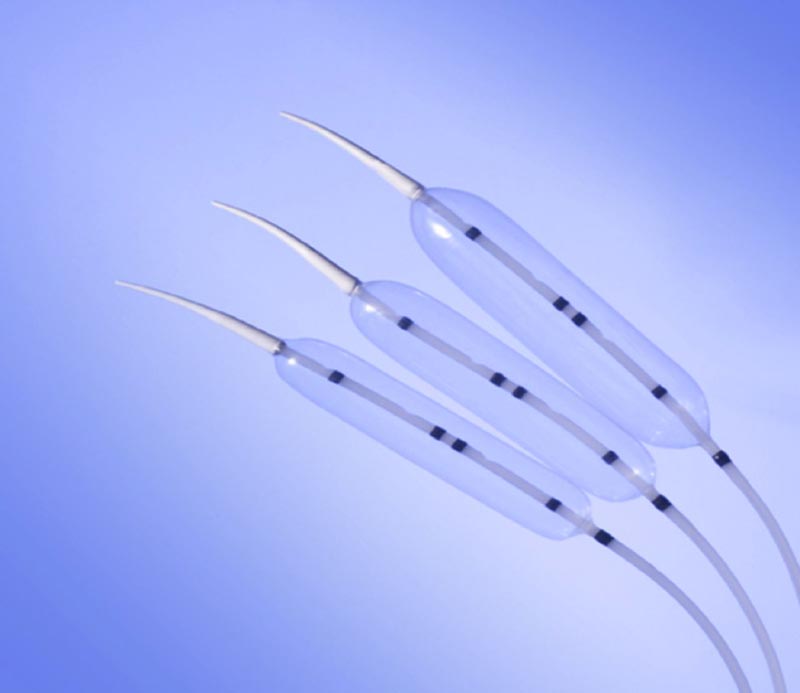
• Pneumatic expansion
Pneumatic dilation is a radioscopic procedure performed with a high-caliber, air-filled balloon for tearing the muscle fibers of the LES and is an established and well-validated treatment for achalasia. Before the arrival of MHL and ITBE, pneumatic dilation was the first intervention performed to avoid open surgery for achalasia. Fifteen retrospective studies with more than 2000 patients and a mean follow-up of up to five years showed a symptomatic response in 71% of patients, with 3% of perforations. 55 Currently, most dilations are performed with the Rigiflex balloon dilator.
This technique is low-cost and effective, although its durability is of concern. In an extensive review of 20 studies with 2497 patients in total, pooled estimates after a single dilation showed 60%, 59%, 55%, and 25% of patients in symptomatic remission at one, two, three, and five years, respectively. .56 In four studies in which patients had two or more dilations at the initial session, 92%, 84%, 78%, and 64% were in remission at those time points.56
The perforation rate was 4% in this group and 2% in patients in the single dilation group. Several studies evaluated the effect of repeated dilations, with a larger balloon every two to three weeks until remission was achieved or until resting LES pressure was <15 mm. The initial remission rate was 91%, with five- and 10-year remission rates of 97% and 93%, while it was 67% and 50%, respectively, when a single dilation was performed.57
Complications with this technique are rare. Perforation occurs in around 2% of procedures and is associated with the first dilation, with difficulty keeping the balloon in the correct position and with a balloon larger than 30 mm.67 68
• Heller myotomy
Ernest Heller performed the first successful surgical myotomy for achalasia in 1913.69 In its various modalities, surgical myotomy is an excellent option and, until the creation of POEM, the gold standard method due to its reliability and durability. It is currently performed laparoscopically (LLM), and recent emphasis has been placed on extending the myotomy 2-3 cm into the proximal stomach to further reduce LES pressure (optimally to <10 mm Hg) and the tendency to dysphagia.70 Extended myotomy increases the risk of GERD and the current consensus is to add a partial fundoplication to reduce this risk.71
Meta-analysis of more than 3000 patients undergoing MHL observed excellent relief (decrease in Eckardt score to ≤3) in 89.3% of patients, with an average follow-up of up to 35 months.51 Young men with pressures very high LES are particularly suitable candidates for MHL. The effectiveness of myotomy decreases over time.
In one series, the response measured by the Eckardt score decreased from 89% at six months to 57% at six years.72 Complications include esophageal perforation (7-15%).67 and the most common is GERD (10-40%). Partial Dor or Toupet fundoplications can loosen over time and patients often require proton pump inhibitors.73
• Comparative analysis
≈ Pneumatic dilation vs ITBE : The general consensus is that pneumatic dilation is more effective than ITBE in patients with achalasia, especially over time.74-78 This was confirmed in a meta-analysis of seven studies in 2014, which found no significant differences in post-treatment LES pressures or clinical scores at one month, but notable differences at six months in favor of pneumatic dilation, an even more notable difference at one year ( P <0.001).79
≈ MHL vs ITBE . In a high-quality, randomized controlled study (40 patients in each group), symptomatic improvement was comparable at six months, but a greater proportion of patients undergoing MHL were asymptomatic at two years (88% v 34 %; P <0.05).80
≈ Pneumatic dilation vs surgical myotomy . In four randomized controlled trials 16-84 progressive pneumatic dilation was more likely to keep patients free of dysphagia. Csendes observed that 65% of patients with pneumatic dilation had a good response at 58 months, while 95% of patients with MHL at 62 months had an excellent response.85. In Boeckxstaens’ study, the therapeutic success of pneumatic dilation was 90% at one year and 86% at two years, not significantly different from that of MHL patients with Dor fundoplication. The pneumatic dilation group had significant complications.84
A meta-analysis published in 2013 evaluated 161 studies and found only three randomized controlled studies of patients with newly diagnosed achalasia who were randomized into two groups: gradual pneumatic dilation or not and MHL. The response at one year was significantly better for MHL than for pneumatic dilation (86% v 76%).66. A large comparative study found similar responses at six months, but a significantly better response at six years for those who had undergone MHL (57% v 44%).72
People with achalasia often receive multiple treatments throughout their lives. MHL is usually performed if pneumatic dilation fails and vice versa.83 90
• Other treatments
Other treatments that are not widely accepted are transcutaneous electrical nerve stimulation, stents , and sclerosing injection of ethanolamine into the LES.91-93
► POEM
POEM is a fortunate offshoot of research into a submucosal tunnel technique to allow “scarless” transluminal endoscopic access to the mediastinum through the esophageal wall when performing procedures that are traditionally done through skin incisions (such as mediastinoscopy and lymph node biopsy).98 99
Haruhiro Inoue performed the first modern myotomy in humans in Japan in 2008 using the submucosal tunnel technique.101 He also coined the acronym POEM for the procedure. The Natural Orifice Surgery Consortium for Advancement and Research (NOSCAR) sponsored an international survey of pioneering centers performing POEM in early 2012. Of the 20 centers, 16 participated in a detailed survey that covered all aspects of POEM.103
Based on the excellent results reported by these pioneering centers the use of POEM continued to grow rapidly throughout the world. In 2015, the NOSCAR POEM report, the ASGE POEM PIVI (preservation and incorporation of valuable endoscopic innovations), was published.104 105
Current publications report that 2000 procedures have already been performed worldwide.
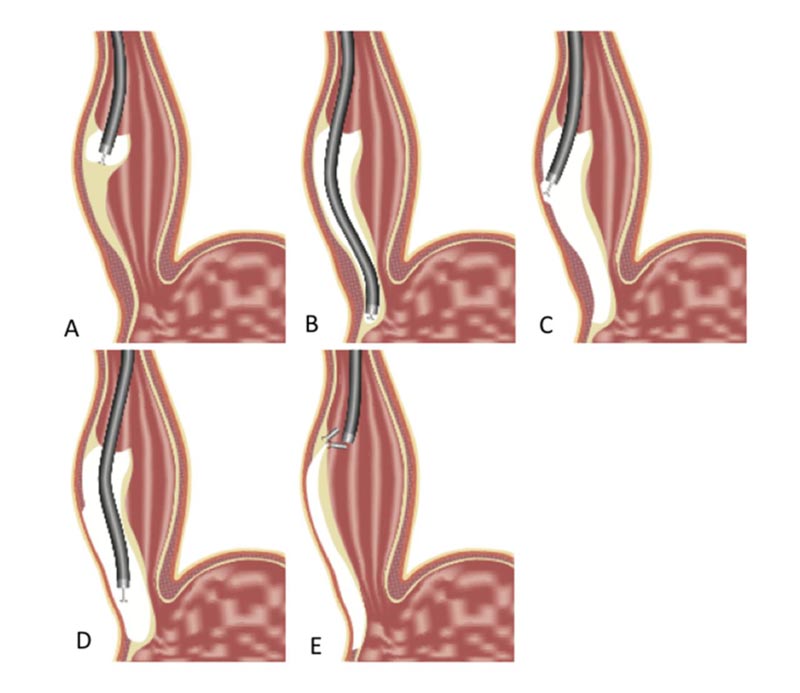
♦ Technique
The flexible endoscope is inserted through the mouth and into the esophagus. With a small electrosurgical scalpel inserted through the endoscope, a small incision is made in the mucosa in the middle part of the esophagus, allowing the endoscope to be inserted into the submucosal space between the mucosa and the muscularis propria, formed by loose connective tissue.101 The submucosal space (usually only 1-2 mm thick) is expanded to about 15 mm by repeated injections of saline to accommodate the endoscope, which has a diameter of 10 mm.
With gradual advancement of the endoscope and dissection of the submucosa with the electrosurgical scalpel, a tunnel is created in the submucosa that extends from the middle part of the esophagus to the gastric cardia. Then, with the endoscope located in this tunnel and starting a few centimeters distal to the mucosal incision, the electric scalpel is used to cut the esophageal muscle and perform a Heller myotomy with a “scarless” endoscopic approach through from a natural orifice.
This is in contrast to the transcutaneous laparoscopic approach, which requires five surgical incisions and extensive abdominal dissection to reach the esophagus. With this technique, closing the 15-20 mm incision that forms the entry site to the submucosal tunnel with a few clips or sutures completely seals the tunnel and isolates the myotomy from the lumen of the esophagus; thus preventing the risk of loss of esophageal contents.
♦ Efficiency
The NOSCAR POEM document provided a comprehensive review and tabulation of results from series published through early 2014.104 These 14 series had a median follow-up of one year or less and many of them were with small numbers of patients (15-30 ).101-118 All but one were single-center prospective studies.117 All measured efficacy with the parameter used over the past two decades—decreasing the Eckardt score to 3 or less.119
Efficacy was excellent (90-100% at 3-12 months), except in the multicenter study, where efficacy was 82% in patients with one year of follow-up.117 This may have been the result of the effect of a curve of learning because this study brought together the first five to 20 patients from each of the included centers.120
Studies have shown that centers need to perform a minimum of 20-40 POEM procedures to become competent,120 121 and about 60 to master this difficult technique.121 A few studies also evaluated effectiveness using the timed esophagram,114-124, a method more objective than the Eckardt score, and confirmed the good results. In the last two years, publications with follow-up of one year or more appeared in several centers in the USA with 100, 41, 93 and 100 patients, with success rates of 92%, 93%, 96%, 94%, respectively.121- 124
In a study published last year,126 from three centers, with 79 patients and two years of follow-up, a great initial success of 94% at three to six months was shown, which decreased to 88% at 12-18 months and 78% % at two years or more.117 As in the multicenter study mentioned, these more modest results were attributed to the learning curve effect because half of the failures were in the first 10 patients at each center.
In the largest POEM series to date, Inoue et al reported results in 500 patients, with 105 of them having more than three years of follow-up.127 The procedure was technically successful in all cases. Moderately adverse effects occurred in 3.2%, including pneumothorax, hemorrhage, mucosal lesions, postoperative hematomas, pleural effusion, and inflammation of the lesser omentum. No serious adverse events were recorded.
Two-month results showed significant reductions in Eckardt scores and LES pressures. The improvement of the Eckardt score was achieved in 91.7%. On endoscopy, 65% had signs of reflux esophagitis, but only 17% of patients reported symptoms of GERD. At three years, good results were 88.5%, with symptomatic GERD in 21% and signs of reflux esophagitis in 56%. Reflux symptoms were effectively treated with proton pump inhibitors.127
As the authors already noted in another article,128 there are several limitations .
First, there are significant differences between Asian and Western series. For example, the patient population was significantly younger (more than a decade) in Inoue’s works. 129In addition, there were much less difficult patients, such as those previously treated with Botox or Heller (1% and 2% respectively in Inoue’s series compared to 21% with previous Botox and 16% with previous Heller in the series of the authors of this article) and large esophageal dilation greater than 6 cm in esophageal diameter (4% in Inoue vs 27% in the authors’ work).
Second, Inoue used a different definition of efficacy (post-POEM Eckardt <2 or decrease in Eckardt score by ≥4 points) that differs from the definition used by all other published POEM series and most MHL series. (i.e., decrease in Eckardt score to ≤3).
Third, a significant amount of data was missing—for example, although more than 105 patients were more than three years past their POEM, Eckardt score data were only present in 58% and follow-up endoscopy only in 15%. %.
Some recent publications have focused on the results of POEM in certain patient groups in whom the procedure may be preferable to MHL.
First, patients with achalasia type III, “spastic” achalasia, require a long myotomy in the esophageal body that cannot be performed with a laparoscopic approach, but can be easily performed through the peroral approach. A recent multicenter study showed excellent results after POEM in patients with spastic esophageal disorders, with clinical improvement in 93% of patients during a mean follow-up of 234 days. 130
Second, in children six small studies showed excellent results after POEM, similar to those in adults and similar to the results of laparoscopic Heller myotomy in children, but with a much less invasive procedure than this.131-137
Third, patients with advanced achalasia often require esophagectomy. Because POEM does not leave a periesophageal scar or adhesions, it is preferred to MHL, which does not prevent the need for esophagectomy and can cause scars that subsequently make esophagectomy difficult. In a recent prospective study of 32 patients with advanced achalasia undergoing POEM, 96% of cases were successful at 30-month follow-up (mean decrease in Eckardt score from 7.8 to 1.4; P < 0.001).138
Fourth, patients who have previously received treatment with Heller myomectomy, botox, or balloon dilation are candidates for POEM. 139,140-142
♦ Adverse effects
The incidence of serious adverse events after POEM is low and no deaths have been reported. Some minor adverse effects143 are:
• Small accidental mucosal lesions over the submucosal tunnel that are easily closed with endoscopic staples during the procedure.
• Pneumomediastinum, pneumothorax, pneumoperitoneum, or tight pneumoperitoneum during the procedure easily resolved with an angiocath or Veress needle
• Intraprocedural hemorrhage that is controlled through endoscopic hemostasis.
These incidents occur in 10-25% of cases,103-105 and their incidence decreases with experience.121
Intra- and periprocedural adverse effects of moderate severity143 are aspiration of lumen contents (usually during intubation) and symptomatic pneumothorax requiring drainage.144 Late adverse effects usually occur 24-48 hours after the procedure. They are of moderate severity, such as bleeding that requires a new endoscopy for hemostasis,122-145 and rarely, in severe cases, surgical intervention or tamponade with a Blakemore balloon.146
Other late adverse effects include tunnel closure dehiscence122 and cardiopulmonary problems, such as pneumonia147 or atrial fibrillation.148 All published works reported low rates of adverse effects (<2-3%), except for a 2010 Chinese paper that reported adverse effects. in more than 50% of patients, mainly pneumothorax.144 The authors attributed this to the use of air instead of carbon dioxide, which is absorbed about 170 times faster from body cavities than air. After this Chinese center, which performed the most POEM procedures in the world (>1700), switched to carbon dioxide, the rate of adverse effects decreased to the figures of other centers. Currently, POEM is a very safe procedure in expert hands.
♦ GERD after POEM
The problem of GERD after POEM is of great interest because POEM is rapidly displacing MHL as the first-line treatment for achalasia. GERD was not initially recorded after POEM, 101-107 probably because there was a reliance on symptom scores or unstructured interviews. When systematic objective evaluation with endoscopy to evaluate for reflux esophagitis and pH studies to measure acid exposure began, it was evident that the rate of GERD after POEM was much higher than previously thought. 115-151
Studies found that 27-59% of patients had endoscopic signs of GERD after POEM, 29-38% had excessively increased acid exposure on pH studies, and 15-23% suffered from frequent GERD symptoms. These patients were effectively treated with proton pump inhibitors. As already mentioned, patients with achalasia may have false-positive pH studies due to stasis and fermentation of retained food, with production of lactic acid.15 16.
The widespread belief is that the more effective the tearing of the LES muscle fibers, the more effective the relief of dysphagia will be, but at the cost of a greater risk of GERD. Because of this, most specialists believe that during POEM or MHL, the effectiveness of the myotomy cannot be jeopardized in an attempt to reduce the incidence of GERD. This is because GERD can be easily detected and treated, whereas persistent dysphagia and impaired esophageal emptying after MHL or POEM pose a much more difficult diagnostic and therapeutic problem. Is
It is important to note, however, that GERD can be asymptomatic in 40-50% of cases.122 151 It is therefore necessary after POEM, at least a postoperative pH study and endoscopic surveillance every one or two years. to detect patients with GERD to treat them and prevent reflux complications, such as Barrett’s esophagus and peptic strictures.
However, if for any reason Dor or Toupet fundoplication is necessary, POEM does not interfere with these procedures.
♦ POEM in relation to usual treatments
The recent ASGE PIVI reviewed the results of routine and POEM treatments in detail and proposed the following efficacy and safety thresholds for the adoption of POEM:
• At least 80% efficacy at 12 months (defined as Eckardt score ≤3 with a dysphagia component of ≤2)
• Serious adverse event rate of 6% or less
• 30-day mortality of 0.1% or less.105
Based on the data published so far, POEM results exceed these thresholds. There are currently no randomized studies of POEM versus standard treatments.
Three retrospective cohort studies from the US compared MHL with POEM.109-158 The first compared 18 POEM procedures with 55 MHL and found that POEM was faster (113 v 125 min; P < 0.05), with less bleeding (10 v 55 ml; P <0.001), but that the adverse effects and hospitalization time were similar for both techniques.
The second study compared 18 POEM procedures with 21 MHL and found similar adverse effects, but less postoperative pain and a quicker return to activities of daily living after POEM (2.2 vs. 6.4 days; P =0.03 ).
The third study compared 37 POEM procedures with 64 MHL and found similar adverse effects (one serious effect in each group). POEM had a shorter duration of the procedure (120 vs 160 min; P <0.001), shorter hospitalization time (1.1 vs 2.5 days; P <0.001), better Eckardt score at one month (0.8 vs 1. 8; P <0.001) and six months (1.2 vs 1.7; P =0.1) and significantly less dysphagia in response to solids at six months (0% vs 29% of patients with dysphagia with solids per at least weekly; P <0.001). The study also obtained pH data for 23 POEM and 31 MHL and found similar rates of GERD (POEM 39% vs LHM 32%; not significant).
These studies found that POEM was equivalent or superior to MHL in all areas evaluated.
Based on these comparative data and the excellent results of POEM in more than 20 published prospective series and taking into account that MH is more invasive, any attempt at a randomized study between MHL and POEM is unlikely to recruit an adequate number of patients. A more feasible and clinically important investigation would be to compare POEM with pneumatic dilation, which has the advantages of being a simpler outpatient procedure, although at the cost of less durability and requiring more interventions over time.
► RECOMMENDATIONS
The recommendations for achalasia from the main scientific societies of gastroenterology are already three or four years old and do not include recent therapeutic advances. The recommendations of the Society of American Gastrointestinal and Endoscopic Surgeons of 2012 159 and the American College of Gastroenterology of 2013 40 advise suspecting achalasia in patients with dysphagia with solids and liquids with regurgitation that does not respond to proton pump inhibitors.
Endoscopy is necessary to rule out mechanical obstruction and pseudoachalasia, esophagography to evaluate emptying, and manometry to confirm the diagnosis. Treatment should be carried out according to age, sex, patient preference and institutional experience. In general, definitive treatment (pneumatic dilation or myotomy) is recommended. ITBE is reserved for patients who are not good candidates for definitive treatment. Post-treatment follow-up with the Eckardt score (subjective score) and esophagography (objective test) is recommended.
There are no clear recommendations regarding surveillance endoscopy for esophageal cancer and disease progression. Some specialists recommend endoscopic or radiological surveillance every three years in patients with achalasia for more than 10-15 years.
► CONCLUSIONS
Achalasia is a rare disorder of esophageal mobility, mainly manifesting with dysphagia. Recently the paradigm for its diagnosis and treatment changed. High-resolution manometry allowed the accurate diagnosis of achalasia, its differentiation from other similar diseases, and the classification of achalasia into subtypes.
Medical treatment is ineffective for achalasia. Until 2008, treatment was limited to pneumatic dilation, botulinum toxin injection, and MHL. Over the past six years, prospective studies with short-term and intermediate-term results have shown that the POEM procedure is effective and safe and represents an important advance in the treatment of achalasia because it combines the superior efficacy of MHL with the relative ease and non-invasive nature of endoscopy.
POEM has been successful in all subtypes of achalasia and in patients who had previously undergone Heller esophagomyotomy, pneumatic dilation, or ITBE. Patients treated with MHL or POEM should have their pH closely monitored, since GERD is the most common adverse effect after both procedures and proton pump inhibitors are usually necessary. Endoscopy should be performed periodically due to the increased risk of cancer associated with GERD and achalasia. Comparative studies are expected between the results obtained from the POEM and those already known from the MHL.
Technological advances in diagnosis and the addition of POEM to the therapeutic armamentarium will benefit patients with achalasia.















