Coronavirus disease 2019 (COVID-19) is increasing rapidly among young adults in the US. Often described as a disease that affects older adults, to our knowledge, few studies have included younger patients to better understand your anticipated clinical trajectory.
We investigated the clinical profile and outcomes of 3,222 young adults (defined by the US Census as ages 18 to 34 years) who required hospitalization for COVID-19 in the US.
Methods
Young adults aged 18 to 34 years with the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) code U07 (COVID-19, virus identified) discharged between April 1 and April 30 were identified. June 2020 in the Premier Healthcare Database, an all-payer hospital database that includes 1,030 U.S. hospitals and healthcare systems and more than 8 million annual hospital admissions
Pregnant young adults (n = 1644) were excluded because many were admitted for delivery and not for COVID-19 infection. Only a patient’s first hospitalization for COVID-19 was considered.
Comorbidities and outcomes during COVID-19 hospitalization were defined using ICD-10 diagnosis, procedure, or billing codes .
Intensive care utilization was defined by a billing code for the intensive care unit room or daily ventilator management.
Independent factors associated with the composite outcome of mechanical ventilation or death were identified using multivariable logistic regression.
Participating hospitals reported on race and ethnicity.
Data were collected and de-identified by Premier and transferred and analyzed at Brigham and Women’s Hospital using Stata, version 14 (StataCorp). The Mass General Brigham institutional review board approved the study protocol; The requirement for informed consent was waived due to the de-identified nature of the data. A two-sided p value of <0.05 was considered significant.
Results
Among 780,969 adults discharged between April 1, 2020 and June 30, 2020, 63,103 (8.1%) had the ICD-10 code for COVID-19, of whom 3,222 (5%) were non-pregnant young adults (ages 18-34) admitted to 419 US hospitals
The mean (SD) age of this population was 28.3 (4.4) years ; 1,849 (57.6%) were men and 1,838 (57.0%) were black or Hispanic.
In total, 1187 (36.8%) had obesity, 789 (24.5%) had morbid obesity, 588 (18.2%) had diabetes, and 519 (16.1%) had hypertension (table).
During hospitalization
- 684 patients (21%) required intensive care .
- 331 (10%) required mechanical ventilation.
- 88 (2.7%) died.
Vasopressors or inotropes were used in 217 patients (7%), central venous catheters in 283 (9%), and arterial catheters in 192 (6%).
The median hospital stay was 4 days (interquartile range, 2-7 days).
Among those who survived hospitalization, 99 (3%) were discharged to a post-acute care facility.
Morbid obesity (adjusted odds ratio [OR], 2.30; 95% CI, 1.77-2.98; vs. no obesity; P < 0.001) and high blood pressure (adjusted OR, 2.36; 95%, 1.79-3.12; P <0.001) were frequent and, in addition to male sex (adjusted OR, 1.53; 95% CI, 1.20-1.95; P = 0.001) were associated with an increased risk of death or mechanical ventilation.
The odds of death or mechanical ventilation did not vary significantly with race and ethnicity.
Morbid obesity was present in 140 patients (41%) who died or required ventilation. Diabetes was associated with an increased risk of this outcome in univariate analysis (OR, 1.82; 95% CI, 1.41-2.36; P < 0.001) but did not reach statistical significance after adjustment (adjusted OR , 1.31; 95% CI, 0.99-1.73; p = 0.06).
Patients with multiple risk factors (morbid obesity, hypertension, and diabetes) faced similar risks to 8,862 middle-aged non-pregnant adults (35-64 years) with COVID-19 infection without these conditions (Figure).
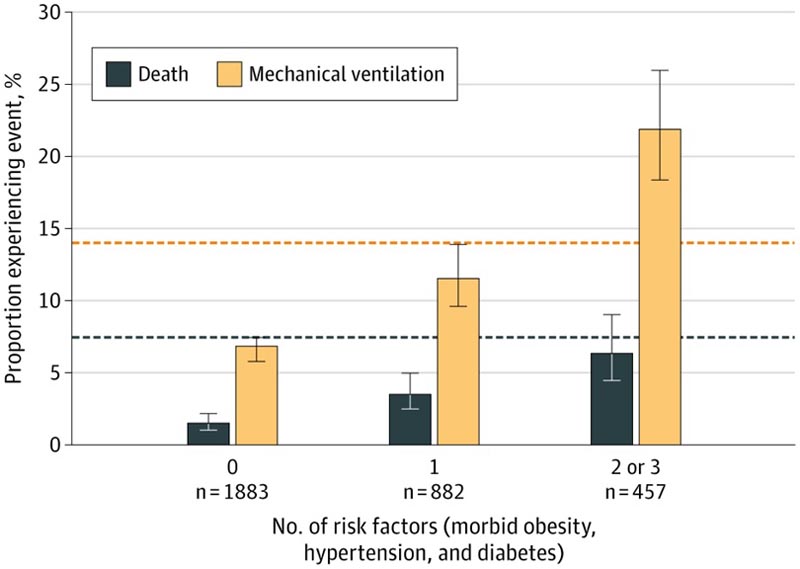
Morbid obesity, diabetes, and hypertension were determined using International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes during coronavirus 2019 (COVID-19) admission. The proportions of patients who experienced death and mechanical ventilation were compared to a reference group of 8,862 middle-aged (35-64 years) non-pregnant patients with COVID-19 without either of these conditions in the Premier database (dotted lines ). Error bars refer to 95% CI.
Discussion
Young adults ages 18 to 34 hospitalized with COVID-19 experienced substantial rates of adverse outcomes:
|
This in-hospital mortality rate is lower than that reported for older adults with COVID-19, but approximately double that of young adults with acute myocardial infarction .
Morbid obesity, hypertension, and diabetes were common and associated with increased risks of adverse events.
Young adults with more than one of these conditions faced risks comparable to those seen in middle-aged adults without them.
More than half of these patients who required hospitalization were black or Hispanic, consistent with previous findings of disproportionate disease severity in these demographic groups.5,6
Limitations of this study included defining COVID-19 infection and comorbidities using ICD-10 codes, which may be subject to misclassification and variable reporting of race and ethnicity across hospitals.
The definition of COVID-19 infection did not require microbiological confirmation.
Given the marked increase in COVID-19 infection rates in young adults, these findings underscore the importance of infection prevention measures in this age group.
















