Despite two decades of research, outcomes after heart failure hospitalizations remain poor. Countless interventions have been studied, but most have failed to consistently improve outcomes. For example, tools for stratifying risk exist , but their effect has been limited by modest predictive performance and uncertainty regarding the best way to modify risk. Early follow-up after hospital discharge is recommended as a strategy to improve outcomes, but has not achieved wide acceptance, in part due to limited resources.
Background
Patients with acute heart failure are frequently or systematically hospitalized, often because the risk of adverse events is uncertain and options for rapid follow-up are inadequate. It is not yet known whether using a strategy to help doctors make decisions about discharging or admitting patients, along with rapid follow-up in an outpatient clinic, would affect the results.
Methods
In a stepped, cluster-randomized trial conducted in Ontario, Canada, we randomly assigned 10 hospitals to staggered start dates for one-way crossover from the control phase (usual care) to the intervention phase, which involved the use of an algorithm at the point of care to stratify patients with acute heart failure according to risk of death.
During the intervention phase, low-risk patients were discharged early (within ≤3 days) and received standardized outpatient care, and high-risk patients were admitted to the hospital.
The co-primary outcomes were a composite of death from any cause or hospitalization for cardiovascular causes within 30 days of presentation and the composite outcome within 20 months.
Results
A total of 5452 patients were enrolled in the trial (2972 during the control phase and 2480 during the intervention phase).
Within 30 days , death from any cause or hospitalization for cardiovascular causes occurred in 301 patients (12.1%) who enrolled during the intervention phase and in 430 patients (14.5%) who enrolled during the intervention phase. control phase (adjusted hazard ratio, 0.88; 95% confidence interval [CI], 0.78 to 0.99; P = 0.04).
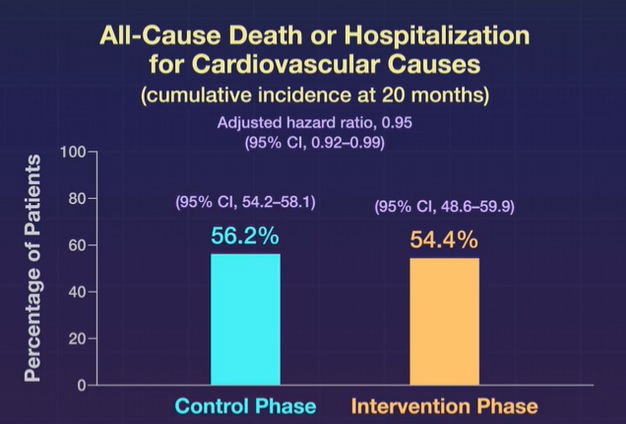
Within 20 months , the cumulative incidence of primary outcome events was 54.4% (95% CI, 48.6 to 59.9) among patients who enrolled during the intervention phase and 56.2% (95% CI, 48.6 to 59.9) among patients enrolled during the intervention phase. % (95% CI, 54.2 to 58.1) among patients who enrolled during the control phase (adjusted hazard ratio, 0.95; 95% CI, 0.92 to 0.99) .
Conclusions Among patients with acute heart failure seeking emergency care, use of a hospital-based strategy to support clinical decision making and rapid follow-up led to a lower composite risk of death from any cause or hospitalization for cardiovascular causes within 30 days than usual care. |
(Funded by Ontario SPOR Support Unit and others; COACH ClinicalTrials.gov number, NCT02674438. opens in new tab.)
















