Summary We report temporal patterns of viral shedding in 94 patients with laboratory-confirmed COVID-19 and modeled COVID-19 infectivity profiles from a separate sample of 77 infectious-infected transmission pairs. We observed the highest viral load in throat swabs at the time of symptom onset, and inferred that infectivity peaked at or before symptom onset . We estimate that 44% (95% confidence interval, 25-69%) of secondary cases were infected during the presymptomatic stage of index cases, in settings with substantial family clustering, active case finding, and out-of-home quarantine. Disease control measures should be adjusted to take into account the likely substantial presymptomatic transmission. |
Major
SARS-CoV-2, the causative agent of COVID-19, spreads efficiently, with a basic reproductive number of 2.2 to 2.5 determined in Wuhan1,2. The effectiveness of control measures depends on several key epidemiological parameters (Fig. 1a), including the serial interval (duration between the onset of symptoms of successive cases in a chain of transmission) and the incubation period (time between infection and onset of symptoms).
The variation between individuals and chains of transmission is summarized in the incubation period distribution and the serial interval distribution, respectively. If the average observed serial interval is shorter than the average observed incubation period, this indicates that a significant portion of transmission may have occurred before infected individuals have developed symptoms .
Significant presymptomatic transmission would likely reduce the effectiveness of control measures initiated by the onset of symptoms, such as isolation, contact tracing, and improved hygiene or mask use for symptomatic people.
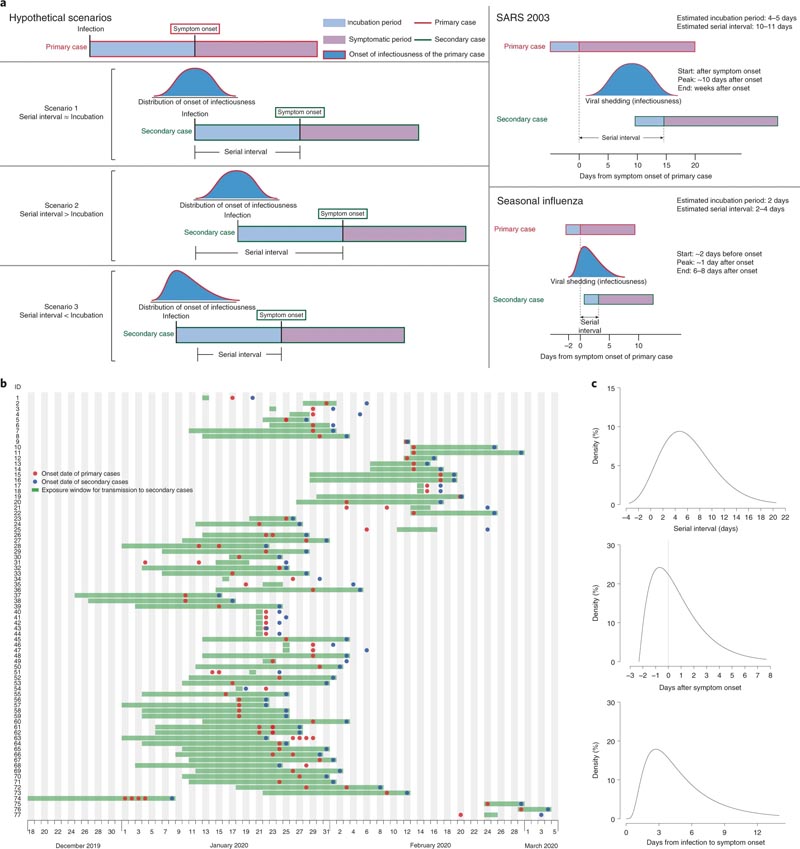 a, Scheme of the relationship between different time periods in the transmission of infectious diseases. b, pairs of human-to-human transmission of the SAR-CoV-2 virus (N = 77). We assumed a maximum exposure window of 21 days before the onset of symptoms in secondary cases. Detailed information on transmission pairs and source of information is summarized in Supplementary Tables 2 and 3. c, Distribution of estimated serial interval (top), inferred infectiousness profile (middle), and assumed incubation period (bottom) of COVID-19.
a, Scheme of the relationship between different time periods in the transmission of infectious diseases. b, pairs of human-to-human transmission of the SAR-CoV-2 virus (N = 77). We assumed a maximum exposure window of 21 days before the onset of symptoms in secondary cases. Detailed information on transmission pairs and source of information is summarized in Supplementary Tables 2 and 3. c, Distribution of estimated serial interval (top), inferred infectiousness profile (middle), and assumed incubation period (bottom) of COVID-19.
SARS (severe acute respiratory syndrome) was notable because infectivity increased around 7 to 10 days after symptom onset3,4. Onward transmission can be substantially reduced by containment measures such as isolation and quarantine (Fig. 1a) 5. In contrast, influenza is characterized by an increase in infectiousness shortly before or even before the onset of symptoms6.
In this study, we compared clinical data on virus shedding with separate epidemiological data on incubation periods and serial intervals between cases in chains of transmission, to draw inferences about infectiousness profiles.
Among 94 patients with laboratory-confirmed COVID-19 admitted to Guangzhou Eighth Hospital, 47/94 (50%) were men, the mean age was 47 years, and 61/93 (66%) were moderately ill (with fever and/or or respiratory symptoms and radiographic evidence of pneumonia), but none were classified as "severe" or "critical" on hospital admission.
A total of 414 throat swabs were collected from these 94 patients, from the onset of symptoms to 32 days after onset. We detected high viral loads soon after symptom onset, which then gradually decreased toward the limit of detection around day 21 . There were no obvious differences in viral loads between sex, age groups, and disease severity (Fig. 2).
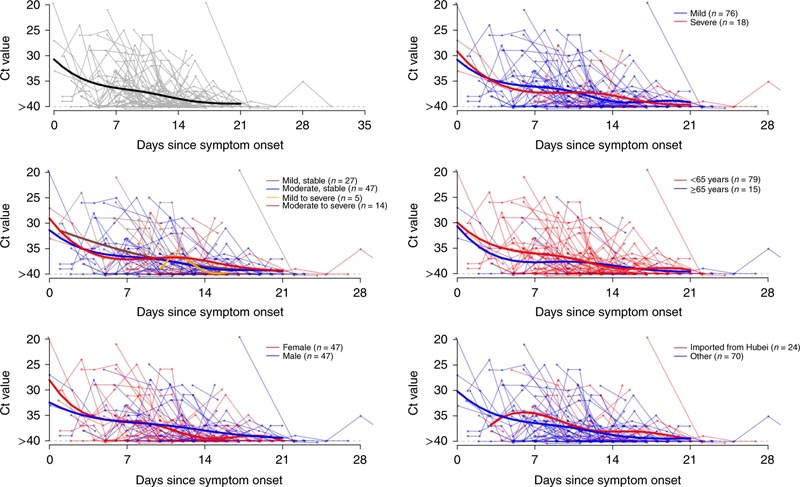
Viral load (threshold cycle (Ct) values) detected by RT – PCR (reverse transcription PCR) in throat swabs from patients infected with SARS-CoV-2 (N = 94), overall and stratified by disease severity , sex, age group and link to Hubei province. The detection limit was Ct = 40, which was used to indicate negative samples. Thick lines show the trend in viral load, using smooth splines. We added some noise to the data points to avoid overlaps.
Separately, based on 77 transmission pairs obtained from publicly available sources inside and outside mainland China the serial interval was estimated to have a mean of 5.8 days (95% confidence interval (CI), 4.8 – 6.8 days) and a median of 5.2 days (95% CI, 4.1 to 6.4 days) based on a fitted gamma distribution, with negative serial intervals of 7.6% (Fig. 1c ).
Assuming an average incubation period distribution of 5.2 days from a separate study of early COVID-19 cases,1 we infer that infectivity began from 2.3 days (95% CI, 0.8-3.0 days) before symptom onset and it peaked at 0.7 days (95% CI, −0.2–2.0 days) before symptom onset (Fig. 1c).
The estimated proportion of presymptomatic transmission (area under the curve) was 44% (95% CI, 25-69%). Infectivity was estimated to decline rapidly within 7 days. Viral load data were not used in the estimation, but showed a similar monotonic decreasing pattern.
| In the sensitivity analysis, using the same estimation procedure but keeping the onset of infectiousness constant from 1 to 7 days before the onset of symptoms, it was shown that infectivity peaks at 0-2 days before the onset of symptoms. of symptoms, and the proportion of presymptomatic transmission ranged from 46% to 55%. |
Finally, simulation showed that the proportion of short serial intervals (e.g., <2 days) would be higher if infectiousness was assumed to begin before symptom onset. Given the 7.6% negative serial intervals estimated from the paired infector-infected data , the onset of infectivity at least 2 days before onset and the peak of infectivity 2 days before to 1 day after onset would be more consistent with this observed proportion.
Here, we use detailed information on the timing of symptom onset in transmission pairs to infer the infectiousness profile of COVID-19.
We show substantial transmission potential before symptom onset.
Of note, most cases were isolated after the onset of symptoms, avoiding some post-symptomatic transmission. Even higher proportions of presymptomatic transmission of 48% and 62% have been estimated for Singapore and Tianjin, where active case finding was implemented7. Places with active case finding tend to have a higher proportion of presymptomatic transmission, primarily due to rapid quarantine of close contacts and isolation, which reduces the likelihood of secondary spread later in the course of the disease.
In a rapidly expanding epidemic where contact tracing/quarantine and perhaps even isolation are no longer feasible, or in places where cases are not isolated outside the home, we should therefore observe a lower proportion of transmission presymptomatic.
Our analysis suggests that viral shedding may begin 2 to 3 days before the appearance of the first symptoms. After the onset of symptoms, viral loads decreased monotonically, according to two recent studies8,9.
Another study from Wuhan reported that the virus was detected for a median of 20 days (up to 37 days among survivors) after symptom onset10, but infectivity may decrease significantly 8 days after symptom onset as it no longer exists. can be cultivated (according to Wölfel and colleagues11).
Together, these results support our findings that the infectivity profile may more closely resemble that of influenza than SARS (Fig. 1a), although we did not have data on virus clearance before symptom onset6,12. Our results are also supported by reports of asymptomatic and presymptomatic transmission13,14.
For a reproductive number of 2.5, contact tracing and isolation alone are less likely to be successful if more than 30% of transmission occurs before the onset of symptoms, unless >90% of people can be traced. the contacts15. This is more likely to be achieved if the definition of contacts covers 2 to 3 days before the onset of symptoms of the index case , as has been done in Hong Kong and mainland China since late February.
Even when the control strategy is moving away from containment to mitigation, contact tracing would still be an important measure, such as when there are superspreader events that can occur in high-risk settings, including nursing homes or hospitals.
With a substantial proportion of pre-symptomatic transmission, measures such as improved personal hygiene and social distancing for all would likely be the key instruments for community disease control.
Our study has several limitations .
First, the onset of symptoms depends on the patient’s recall after confirmation of COVID-19. The possible recall bias would probably have tended towards the direction of undervaluation, that is, the delay in recognizing the first symptoms. As long as these biases do not differ systematically between the infector and the infected, the serial interval estimate would not be substantially affected. However, the incubation period would have been overestimated and therefore the proportion of presymptomatic transmission was artificially inflated.
Second, shorter serial intervals than those reported here have been reported, but such estimates were lengthened when restricted to infector-infected pairs with more certain transmission links16.
Finally, viral clearance dynamics were based on data from patients who received treatment according to nationally promulgated protocols, including combinations of antivirals, antibiotics, corticosteroids, immunomodulatory agents, and Chinese medicine preparations, which could have modified the dynamic patterns of viral clearance. elimination.
In conclusion , we have estimated that viral shedding from patients with laboratory-confirmed COVID-19 peaked at or before symptom onset, and a substantial proportion of transmission likely occurred before the first symptoms in the index case. More inclusive criteria for contact tracing should be urgently considered to capture potential transmission events 2 to 3 days before symptom onset for effective outbreak control. |