Key points Is male hypogonadism a risk factor for hospitalization due to COVID-19? Findings In this cohort study of 723 men, those with hypogonadism had significantly higher odds than men with eugonadism of being hospitalized, regardless of other known risk factors for COVID-19-related hospitalization. Men who received testosterone therapy had a similar risk of hospitalization as men with eugonadism. Meaning This study suggests that men with hypogonadism are more likely to be hospitalized after COVID-19 infection compared to men with eugonadism and men receiving adequate testosterone therapy. |
The COVID-19 pandemic has taken a heavy toll on public health. Epidemiological data have identified certain characteristics that are associated with adverse outcomes, such as older age, obesity, and systemic diseases, particularly diabetes, hypertension, chronic lung disease, and cardiovascular and cerebrovascular diseases. Additionally, patients hospitalized with COVID-19 are more likely to be men than women. Therefore, it was hypothesized that testosterone is a risk factor for severe COVID-19 and that estrogen may protect against COVID-19.
However, not all men have similar testosterone concentrations. Testosterone concentrations in men decline continuously by 1% to 2% per year beginning in the third decade of life. Additionally, obesity, metabolic syndrome, and chronic diseases such as type 2 diabetes, kidney failure, and chronic lung disease are associated with lower serum testosterone concentrations among men. Thus, aging and the presence of comorbid conditions, which are risk factors for COVID-19 hospitalization, are also associated with hypogonadism, raising the question of whether hypogonadism is a risk factor for COVID-19-related hospitalization. between men.
Recent studies have shown that testosterone concentrations during hospitalization are lower in men with severe COVID-19 than in men with a milder disease course. Because acute illness can reduce testosterone concentrations, it was unclear whether testosterone concentrations in men with severe illness were lower than normal even before they contracted COVID-19. Men with chronically low testosterone concentrations have less muscle mass and less strength, which contributes to reduced lung capacity and ventilator dependence. It is still unknown whether pre-COVID-19 testosterone concentrations in men are associated with disease course after COVID-19.
We reviewed the medical records of men who had a history of COVID-19 infection and had testosterone concentrations measured in the outpatient setting (when they did not have COVID-19). We hypothesized that men with subnormal testosterone concentrations prior to COVID-19 infection would be more likely to require hospitalization than men with normal testosterone concentrations. We also investigated whether testosterone therapy (TTh) modified the risk of hospitalization among men with hypogonadism.
Importance
Male sex is associated with severe COVID-19. It is not known whether the risk of hospitalization differs between men with hypogonadism, men with eugonadism, and those receiving testosterone therapy (TTh).
Aim
To compare COVID-19 hospitalization rates for men with hypogonadism who were not receiving TTh, men with eugonadism, and men receiving TTh.
Design, environment and participants
This cohort study was conducted at 2 large academic health systems in St Louis, Missouri, among 723 men with a history of COVID-19 who had testosterone concentrations measured between January 1, 2017 and December 31, 2017. 2021.
Exhibitions
The main exposure was gonadal status (hypogonadism, eugonadism, and TTh). Hypogonadism was defined as a total testosterone concentration below the limit of normality provided by the laboratory (which ranged from 175 to 300 ng/dL [to convert to nanomoles per liter, multiply by 0.0347]).
Main results and measures
The primary outcome was the rate of COVID-19 hospitalization. Statistical adjustments were made for group differences in age, body mass index, race and ethnicity, immunosuppression, and comorbid conditions.
Results
Of the 723 study participants (mean [SD] age, 55 [14] years; mean [SD] body mass index, 33.5 [7.3]), 116 men had hypogonadism, 427 had eugonadism, and 180 were receiving TTh .
Men with hypogonadism were more likely than men with eugonadism to be hospitalized with COVID-19 (52 of 116 [45%] vs. 53 of 427 [12%]; P < 0.001).
After multivariable adjustment, men with hypogonadism were more likely than men with eugonadism to be hospitalized (odds ratio, 2.4; 95% CI, 1.4-4.4; P < 0.003).
Men who received TTh had a similar risk of hospitalization as men with eugonadism (odds ratio, 1.3; 95% CI, 0.7-2.3; P = .35). Men who received inadequate TTh (defined as below-normal testosterone concentrations while receiving TTh) had increased odds of hospitalization compared with men who had normal testosterone concentrations while receiving TTh (multivariable-adjusted odds ratio, 3.5; 95% CI, 1.5-8.6, P = 0.003).
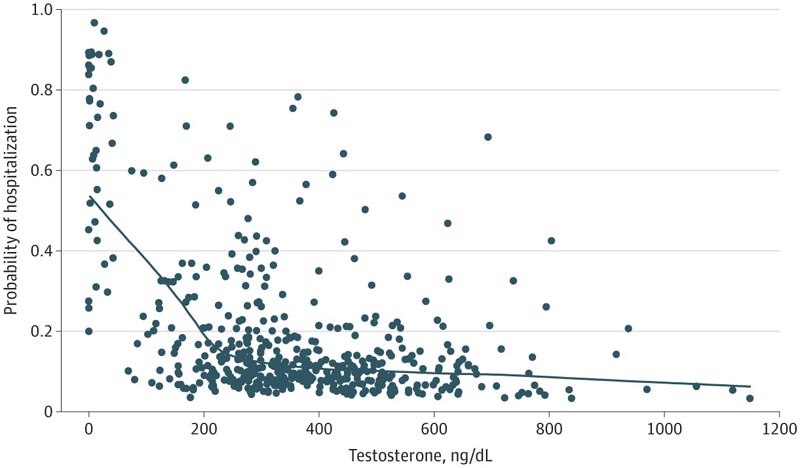
Figure : Probability of hospitalization based on testosterone concentrations in men with hypogonadism and men with eugonadism, after multivariable adjustment for age, body mass index, Charlson comorbidity index, race and ethnicity, and immunosuppression status.
Conclusions and relevance
This study suggests that men with hypogonadism were more likely to be hospitalized after COVID-19 infection compared to those with eugonadism, regardless of other known risk factors. This increased risk was not observed among men who received adequate TTh. Screening and appropriate therapy for hypogonadism should be evaluated as a strategy to prevent severe COVID-19 outcomes among men.
Discussion
We found that men with hypogonadism were 2.4 times more likely than men with eugonadism to be hospitalized if they contracted COVID-19. This increased risk was independent of other factors that increase the risk of COVID-19 hospitalization, such as older age, comorbid conditions, and immunosuppression.
This finding contrasts with the widespread idea that men are more likely than women to be admitted due to COVID-19 because they have higher concentrations of circulating testosterone. In contrast, our data suggest that male hypogonadism is a risk factor for COVID-19 hospitalization.
Final message The findings of this cohort study suggest that men with hypogonadism are more likely than men with eugonadism to be hospitalized after COVID-19 infection. They also suggest that men with hypogonadism who receive adequate TTh to achieve normal testosterone concentrations have a reduced risk of COVID-19-related hospitalization. Prospective clinical trials are needed to explore the efficacy of TTh in preventing hospitalizations after COVID-19 and similar respiratory illnesses among men with hypogonadism. |