Church attendance and prayer can improve heart health among African American adults, according to a study published in the Journal of the American Heart Association .
Research Highlights:
|
African American adults who reported more frequent participation in religious activities and/or deeper spiritual beliefs were more likely to meet some of the American Heart Association ’s key metrics for cardiovascular health, such as regular exercise, a balanced diet, and blood pressure. normal arterial blood pressure, according to new research published today in the Journal of the American Heart Association , a peer-reviewed, open-access journal of the American Heart Association.
This study is the first to investigate among African Americans the association of a comprehensive set of cardiovascular health behaviors: the American Heart Association’s Life’s Simple 7 metrics (diet, physical activity, and nicotine exposure) and physiological factors (weight, cholesterol , blood pressure and sugar levels) with religious beliefs and spirituality. Life’s Simple 7 metrics , established in 2010, were expanded and renamed to Life’s Essential 8 in June 2022, with sleep added as the eighth component of optimal heart health.
African Americans have poorer overall cardiovascular health than non-Hispanic whites, and death from cardiovascular disease is higher in African American adults than in white adults, according to the 2017 scientific statement " Cardiovascular Health in African Americans " from the American Heart Association .
"Healthcare professionals and researchers must recognize the importance of religious and spiritual influences in the lives of African Americans, who tend to be highly religious," said the study’s lead author, LaPrincess C. Brewer, MD, MPH, preventive cardiologist and assistant professor of medicine at Mayo Clinic in Rochester, Minnesota. “With religious and spiritual beliefs included in our approaches, we can make great strides in fostering relationships between patients and physicians and between community members and scientists to build trust and sociocultural understanding of this population.”
Researchers analyzed responses measuring religiosity (strong religious feelings or beliefs of any religion), spirituality, and Life’s Simple 7 cardiovascular health indicators from surveys and health examinations of 2,967 African American participants in the Jackson Heart Study . The Jackson Heart Study is the largest community-based investigation of cardiovascular disease among U.S. African American adults at a single site. On average, participants were 54 years old when enrolled in the study and 66% were women. The ongoing study, begun in 1998, includes more than 5,000 adults ages 21 to 84 who identify as African American and live in the tri-county area of Jackson, Mississippi.
The researchers grouped participants by religious behaviors (their self-reported levels of attending religious services/Bible study groups, private prayer, and using religious beliefs or practices to adapt to difficult life situations and stressful events, called religious coping in the study); and spirituality (belief in the existence of a supreme being, deity or God).
Religious behavior questions were adapted from the Fetzer Multidimensional Measurement of Religiosity/Spirituality (religious attendance, private prayer) and the Religious Coping Scale (religious coping) instruments. Spirituality measures were adapted from the Daily Spiritual Experience Scale, which assesses ordinary daily experiences in accordance with theistic spirituality (belief in the existence of a supreme being, deity or God and feeling the presence of God, desiring closer union closeness with God, feeling the love of God) and non-theistic spirituality (feeling strength in my religion, feeling deep inner peace and harmony or feeling spiritually touched by creation).
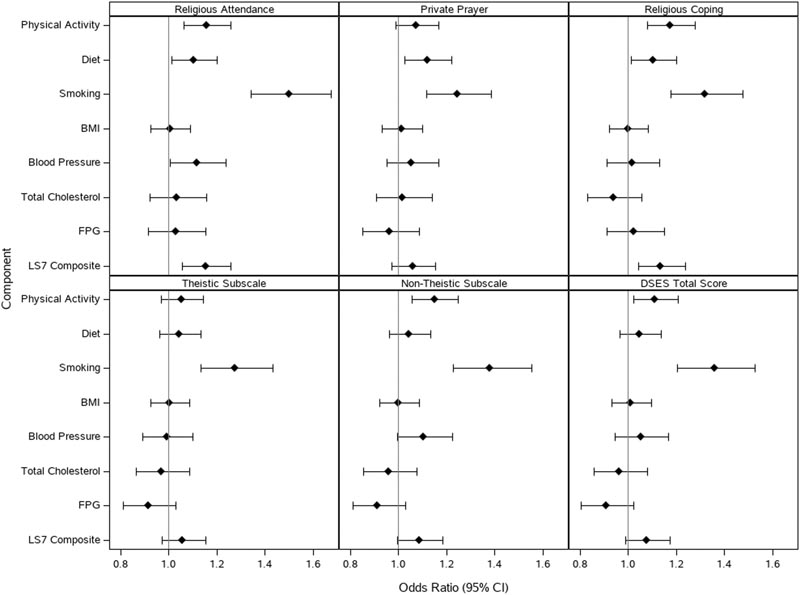
Participants were then grouped according to religiosity and spirituality scores by health factors: physical activity, diet, smoking, weight, blood pressure, blood sugar and cholesterol levels, plus the composite score of the seven components of Life’s Simple 7 to estimate cardiovascular health. The researchers calculated the odds of achieving intermediate and ideal levels of heart disease prevention goals based on religiosity/spirituality scores .
Participants who reported more religious activity or who had deeper levels of spiritual beliefs were more likely to meet key measures for cardiovascular health:
- Greater frequency of attending religious services or activities was associated with a 16% increase in the odds of meeting “intermediate” or “ideal” metrics for physical activity, 10% for diet, 50% for smoking, 12 % for blood pressure and 15% for cardiovascular health composite score.
- Higher reported frequency of private prayer was associated with a 12% increase in the odds of achieving intermediate or ideal diet metrics and a 24% increase in the odds of achieving the smoking-related metric.
- Religious coping was associated with an 18% increased odds of achieving intermediate and ideal levels for physical activity, 10% increased odds for a healthy diet, 32% for smoking, and 14% for the composite score. cardiovascular health.
- Total spirituality was associated with an 11% increase in the odds of achieving intermediate and ideal levels for physical activity and a 36% increase for smoking.
"I was a little surprised by the findings that multiple dimensions of religiosity and spirituality were associated with better cardiovascular health across multiple health behaviors that are extremely difficult to change, such as diet, physical activity, and smoking," Brewer said.
“Our findings highlight the substantial role that culturally tailored health promotion initiatives and lifestyle change recommendations can play in advancing health equity,” he added. “The cultural relevance of interventions may increase the likelihood that they will influence cardiovascular health and also the sustainability and maintenance of healthy lifestyle changes.”
Brewer added, “This is especially important for socioeconomically marginalized communities that face multiple challenges and stressors. “Religiosity and spirituality can serve as stress buffers and serve therapeutic purposes or support self-empowerment to practice healthy behaviors and seek preventive health services.”
The religiosity/spirituality survey was conducted at one point during the Jackson Heart Study , so participants’ cardiovascular health was not analyzed over time. Additionally, people who had known heart disease were not included in this analysis.
Clinical Perspective
What’s new?
In this large cohort of community-dwelling African American adults from the Jackson Heart Study (JHS), the highest levels of religiosity (e.g., religious attendance, private prayer, religious coping) and spirituality (e.g., theistic , nontheistic) were associated with intermediate/nontheistic levels of ideal cardiovascular health across multiple American Heart Association Life’s Simple indicators 7 .
Our study provides the first high-quality corroborating evidence that religiosity and spirituality may have potentially beneficial effects on selected Life’s Simple 7 indicators in African American men and women.
What are the clinical implications?
Recognition by health professionals and researchers of the centrality and influence of religiosity and spirituality in the lives of African American adults may serve as a means to address cardiovascular health disparities through sociocultural understanding and the strategic development of culturally relevant lifestyle interventions.
Co-authors are Janice Bowie, Ph.D., MPH; Joshua P. Slusser; Christopher G. Scott, M.S.; Lisa A. Cooper, MD, MPH; Sharonne N. Hayes, MD; Christi A. Patten, Ph.D.; and Mario Sims, Ph.D., MS Author disclosures are listed in the manuscript.
















