| Covid reinfections are not benign : ~39,000 people with reinfections vs. ~5.4 million controls indicates extensive and persistent risk with a dose-response curve (more risk with repeated reinfections). |
First SARS-CoV-2 infection is associated with an increased risk of acute and post-acute death and sequelae in the pulmonary and extrapulmonary organ systems. However, it is unclear whether reinfection increases the risk incurred after the first infection.
Here we used the US Department of Veterans Affairs national healthcare databases to create a cohort of individuals with first infection (n = 257,427), reinfection (2 or more infections, n = 38,926). and an uninfected control group (n = 5,396,855) to estimate the 6-month risks and burdens of all-cause mortality, hospitalization, and a set of prespecified incident outcomes.
We show that, compared to people with first infection, reinfection contributes to additional risks of all-cause mortality, hospitalization, and adverse health outcomes in the pulmonary and extrapulmonary organ systems (cardiovascular disorders, coagulation disorders, and hematologic disorders). , diabetes, fatigue, gastrointestinal disorders, kidney disorders, mental health disorders, musculoskeletal disorders and neurological disorders); risks were evident in those who were unvaccinated, had 1 injection, or 2 or more injections before second infection; The risks were most pronounced in the acute phase, but persisted in the post-acute phase of reinfection, and most were still evident 6 months after reinfection.
Compared with uninfected controls , assessment of the cumulative risks of repeat infection showed that the risk and burden increased gradually with the number of infections .
The constellation of findings shows that reinfection adds nontrivial risks of all-cause mortality, hospitalization, and adverse health outcomes in the acute and post-acute phase of reinfection.
Reducing the overall burden of death and disease from SARS-CoV-2 will require strategies for reinfection prevention.
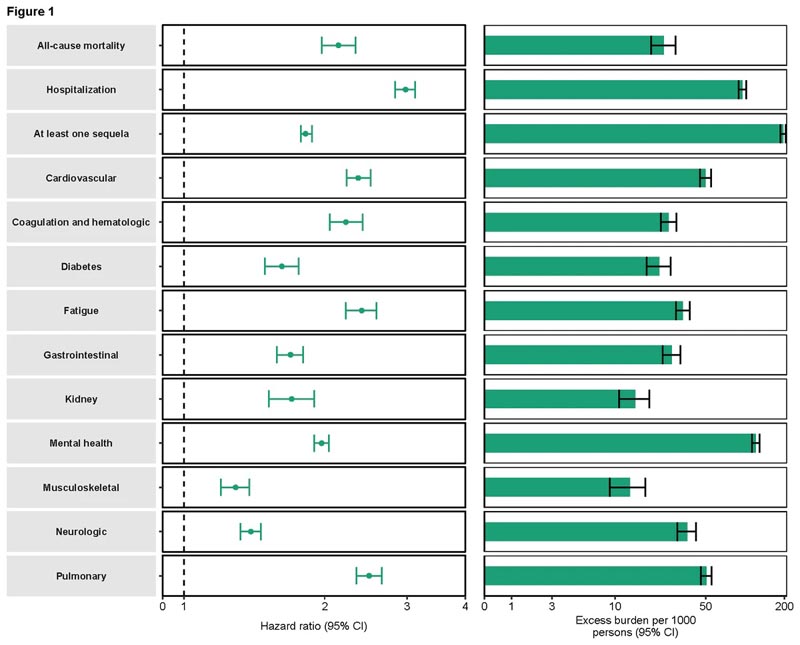
Comparison of people with reinfections vs those with only 1 infection. Consider the doubling of all-cause mortality, adverse cardiovascular and pulmonary outcomes, triple the risk of hospitalization, and the impact on other health domains. The absolute excess load is displayed in the right panel.
Discussion
In this study of 5,693,208 million people, including 257,427 people with first infection, 38,926 people with reinfection, and 5,396,855 uninfected controls, we showed that, compared with people with first infection, people with reinfection exhibited a increased risk of all-cause mortality, hospitalization, and several prespecified outcomes.
The risks were most pronounced in the acute phase, but persisted in the post-acute phase of reinfection, and the risks for most sequelae were still evident at 6 months.
Compared with uninfected controls, assessment of the cumulative risks of repeat infections showed that the risk and burden of all-cause mortality and prespecified health outcomes increased gradually with the number of infections (i.e., risks were lowest in people with 1 infection, increased in people with 2 infections, and highest in people with 3 or more infections).
Taken together, the findings show that reinfection adds non-trivial risks of all-cause mortality and adverse health outcomes in the acute and post-acute phase of reinfection. The findings highlight the consequences of reinfection and emphasize the importance of preventing SARS-CoV-2 reinfection.
In summary , in this study of 5,693,208 we provide evidence that reinfection contributes to additional health risks beyond those incurred in the first infection, including all-cause mortality, hospitalization, and organ system sequelae. pulmonary and extrapulmonary. The risks were evident in the acute and post-acute phase of reinfection.
Evidence suggests that for people who have already had a first infection, preventing a second infection may protect them from additional health risks. Prevention of SARS-CoV-2 infection and reinfection must remain the goal of public health policy.