During the coronavirus disease 2019 (COVID-19) pandemic, reports described fewer hospitalizations, procedures, and visits for cardiovascular (CV) diseases other than COVID-19. After a brief period of ’recovery’, the emergence and rapid spread of the Omicron variant triggered the reintroduction of ’lockdown’ restrictions heralding a future of preparing for and coping with waves of contagion.
Goals
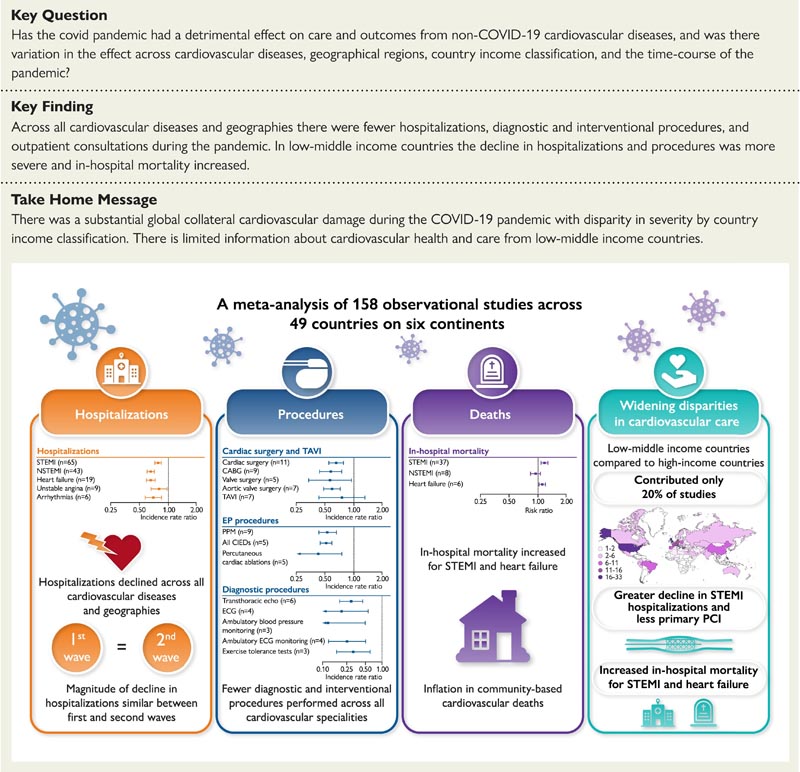
The effect of the COVID-19 pandemic on non-COVID-19 cardiovascular (CV) disease care and outcomes is unknown. A systematic review and meta-analysis was performed to quantify the effect and investigate variation by CV disease, geographic region, country income classification, and the time course of the pandemic.
Methods and results
From January 2019 to December 2021, Medline and Embase databases were searched for observational studies comparing a pandemic and pre-pandemic period in relation to cardiovascular disease hospitalizations, diagnostic and interventional procedures, outpatient consultations and mortality.
Observational data were synthesized using incidence rate ratios (IRR) and risk ratios (RR) for binary outcomes and weighted mean differences for continuous outcomes with 95% confidence intervals. The study was registered with PROSPERO (CRD42021265930).
A total of 158 studies, covering 49 countries and 6 continents, were used for quantitative synthesis. Most studies (80%) reported information for high-income countries (HICs). Across all regions and CV diseases, there were fewer hospitalizations, diagnostic and interventional procedures, and outpatient visits during the pandemic.
By meta-regression, in lower-middle-income countries (LMICs) compared to HICs, the decrease in hospitalizations for ST-segment elevation myocardial infarction (STEMI) (RR 0.79, 95% confidence interval [ CI] 0.66–0.94) and revascularization (RR 0.73, 95% CI: 0.62–0.87) was more severe.
In LMICs, but not HICs, in-hospital mortality was increased for STEMI (RR 1.22, 95% CI 1.10–1.37) and heart failure (RR 1.08, 95% CI 1.04–1 ,12). The magnitude of the decrease in CV hospitalizations did not differ between the first and second waves.
Conclusions
There was substantial global CV collateral damage during the COVID-19 pandemic with disparity in severity by country income classification.
Comments
The cost of COVID-19 on global cardiac services
Around the world, cardiac services were severely disrupted. Heart disease is expected to worsen after the pandemic. The repercussions will be with us for "years to come."
The cost of COVID-19 on global cardiac services
A major study has revealed the “global collateral damage” caused by the disruption of cardiac services by the COVID-19 pandemic. Researchers warn that problems with heart health "... will continue to accumulate unless mitigation strategies are quickly implemented."
In the two years since December 2019, when health systems around the world were under extreme pressure and people feared contracting COVID-19, people who experienced an acute cardiac event, such as a heart attack or heart failure heart disease, were kept away or could not be admitted. to a hospital
The study describes a "substantial overall decrease" in hospital admissions for people suffering from cardiovascular disease. As a result, the number of people dying at home or in the community from heart conditions has increased.
In cases where people received medical help, there was, on average, more than an hour’s delay in getting to the hospital or contacting paramedics. People’s chances of surviving a major heart attack depend on timely and appropriate treatment.
Although the problems identified by the researchers were observed worldwide, they were exacerbated in low- to middle-income countries. Hospitals and clinics there struggled to provide gold standard treatment, in some cases using medications instead of interventional procedures, such as placing a stent in a blocked artery.
The result has been an increase in the death rate among cardiovascular patients in hospitals in low- to middle-income countries, as well as more people dying at home from cardiovascular disease in the UK.
Involving an international team of clinicians and data scientists led by the University of Leeds, the study provides the first global assessment of how cardiovascular services have coped during the pandemic.
The study, "The collateral damage of COVID-19 in cardiovascular services: a meta-analysis," was published in the European Heart Journal . In the review, the research team analyzed data from 189 separate research papers analyzing the impact of COVID-19 on cardiovascular services from 48 countries on six continents and covering a two-year period from December 2019.
Dr Ramesh Nadarajah, British Heart Foundation clinical research fellow at the University of Leeds and lead author of the paper, said: “Heart disease is the leading cause of death in most countries, and analysis shows that during the pandemic, people around the world, people did not receive the cardiac care that they should have received.
“That will have ramifications. The longer people wait to receive treatment for a heart attack, the greater the damage to the heart muscle, leading to complications that can be fatal or cause chronic disease. Health systems must strengthen systems to help support and treat people whose heart conditions will inevitably worsen due to the pandemic. The document provides evidence of that.”
Previous systemic reviews of the impact of COVID-19 on cardiovascular services have presented an "incomplete overview", the researchers say. To address that, they comprehensively investigated a range of cardiac services from hospitalizations, heart disease management, diagnostic procedures, outpatient consultations and mortality rates across all regions. They combined data from multiple studies to put a value on the number of cases hospitals and clinics were seeing compared to the number of cases expected if there were no pandemic.
Data from low- to middle-income countries is sparse and researchers believe their funding understates the true extent of the impact of COVID-19 disruption on cardiac services in low- to middle-income countries.
Dr Samira Asma, Deputy Director-General for Data, Analytics and Delivery for Impact at the World Health Organization (WHO) and one of the authors of the paper, said: “This research shows how the COVID-19 pandemic has disrupted cardiac services at all levels and on all continents , and it would be important to continue studying the impact of this disruption.
“Analysis is revealing that the burden of COVID-19 has fallen disproportionately on low- and middle-income countries and we suspect it will widen the inequality gap in cardiac care health outcomes between high-income countries and developing countries.” low and middle income, where 80% of the world’s population lives. “This underscores the need for universal health coverage and access to quality care, even more so during the pandemic.”
Earlier this month, the WHO published estimates of excess deaths associated with the COVID-19 pandemic, which would include people who were unable to access cardiovascular disease prevention and treatment due to overwhelmed health systems.
During 2020 and 2021, the WHO estimated that there were 14.9 million excess deaths worldwide. Problems with heart health will ’pile up’. In the research article, the authors warn that the disruption of cardiovascular services will leave a legacy that will require immediate action by health administrators.
The researchers said: “Collateral cardiovascular damage from missed diagnoses and delayed treatments will continue to accumulate unless mitigation strategies are quickly implemented. “Deferral of interventional procedures, especially for structural heart disease, leaves many patients at high risk for adverse outcomes.”
Professor Chris Gale, consultant cardiologist and lead author, said: “The implications of the COVID-19 pandemic on cardiovascular care and outcomes will be with us for a long time. “There is little doubt that there will continue to be deaths and illnesses that would not otherwise have occurred. “Urgent measures are needed to address the burden of cardiovascular diseases left by the pandemic.”
Professor Deepak L Bhatt, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital, professor of medicine at Harvard Medical School and senior author of the paper, said: "This analysis really brings to light the substantial impact it has had “The COVID-19 pandemic has had and will continue to have a negative impact on cardiovascular health worldwide.”
Main findings Because of the different way survey statistics were collated, researchers used percentages to compare services. Hospitalizations
Treatment delays On average, it took patients 69 minutes longer to receive medical care for a serious heart attack after the onset of their symptoms. Heart attack management The gold standard treatment for many heart attack patients is insertion of a stent into the blocked artery. In many low- and middle-income countries there was a sharp decline in the performance of such procedures: in only 73% of cases in which the patient had a major heart attack and in 69% of cases in which the patient suffered a less serious heart attack. There was a shift to treating patients with blood-thinning medications. heart operations Globally, there was a 34% drop in heart operations. Interventional procedures Just over half (51%) of implantable electronic devices, such as pacemakers, used to control abnormal heart rhythms were fitted compared to the non-COVID-19 period. Deaths from heart disease
|
Discussion
This systematic review and meta-analysis of the effect of the COVID-19 pandemic on CV services has identified a number of important points.
First, the COVID-19 pandemic witnessed a substantial global decline in hospitalizations for acute CV disease, fewer diagnostic and interventional procedures, and fewer outpatient and community-based visits.
Second, we found no difference in the decrease in hospitalizations for STEMI, NSTEMI, and HF during the second wave compared to the first wave. Third, there is a disparity in the severity of collateral CV damage across geographic and economic boundaries.
In low- and middle-income countries and countries outside of Europe and North America, we observed a more severe decline in hospitalizations and revascularization for STEMI, greater delays in STEMI care pathways with more frequent use of thrombolysis, and a high in-hospital mortality from both STEMI and HF.
Conclusions
This systematic review with meta-analysis provides, to date, the most comprehensive summary of the effect of the COVID-19 pandemic on CV services and people with CV disease.
From 189 articles, we show evidence of fewer hospitalizations, procedures, and consultations with higher mortality among hospital and community populations. We identified disparity by geographic region and country income classification in data availability and the severity of the pandemic’s detrimental effect on CV services, and there is currently insufficient data to fully characterize the effects on CV services in LMICs. Despite this, we provide summary evidence that the COVID-19 pandemic resulted in substantial global collateral CV damage.
















