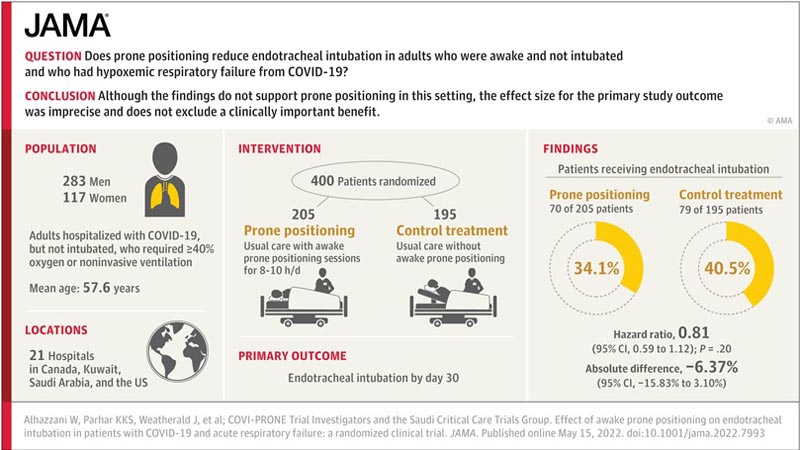
Key points Ask Does prone positioning reduce endotracheal intubation in awake, non-intubated adults who had hypoxemic respiratory failure from COVID-19? Findings In this randomized clinical trial involving 400 adults with acute hypoxemic respiratory failure from COVID-19, awake prone positioning compared to usual care resulted in endotracheal intubation at 30 days in 34.1% vs. 40%. .5% of the participants, respectively. Although the hazard ratio was 0.81, the result was not statistically significant. Meaning Although the findings do not support prone positioning in this setting, the effect size for the primary outcome of the study was imprecise and does not exclude a clinically important benefit. |
Hospitalizations due to COVID-19 strained critical care resources internationally. The surges limited the availability of resources for critically ill patients, emphasizing the need for practical, widely available and affordable interventions. Awake prone positioning emerged as a potentially useful intervention to investigate during the pandemic.
The prone position has been used since the 1970s in patients undergoing invasive mechanical ventilation for acute respiratory distress syndrome. Observational studies demonstrated that prone positioning can result in increased lung volume, homogenized pleural pressure, and reduced shunting.
Additionally, randomized clinical trials found that prone positioning was associated with a lower risk of death in patients undergoing invasive mechanical ventilation for moderate-to-severe acute respiratory distress syndrome (relative risk, 0.74 [95% CI, 0. .56-0.99]).
Awake prone positioning has been widely used for COVID-19 patients. Before the pandemic, there were no randomized clinical trials examining the effects of prone positioning in awake, non-intubated patients with hypoxemic respiratory failure.
The COVI-PRONE ( Awake Prone Position in Hypoxemic Patients with Coronavirus Disease 19 ) trial aimed to evaluate the efficacy and adverse events of awake prone positioning in non-intubated COVID-19 patients with hypoxemic respiratory failure.
Importance
The efficacy and safety of prone positioning is unclear in non-intubated patients with acute hypoxemia and COVID-19.
Aim
To evaluate the efficacy and adverse events of prone positioning in non-intubated adult patients with acute hypoxemia and COVID-19.
Design, scope and participants
Non-blinded, pragmatic, randomized clinical trial conducted in 21 hospitals in Canada, Kuwait, Saudi Arabia, and the USA. Eligible adult patients with COVID-19 were not intubated and required oxygen (≥40%) or non-invasive ventilation.
A total of 400 patients were enrolled between May 19, 2020 and May 18, 2021, and final follow-up was completed in July 2021.
Intervention
Patients were randomly assigned to awake prone position (n = 205) or usual care without prone position (control; n = 195).
Main results and measures
The primary outcome was endotracheal intubation within 30 days of randomization. Secondary outcomes included 60-day mortality, days free from invasive mechanical ventilation or noninvasive ventilation at 30 days, days free from intensive care unit or hospital at 60 days, adverse events, and serious adverse events.
Results
Among the 400 patients who were randomized (mean age, 57.6 years [SD, 12.83 years]; 117 [29.3%] were women), all (100%) completed the trial.
In the first 4 days after randomization, the median duration of prone positioning was 4.8 h/d (IQR, 1.8 to 8.0 h/d) in the awake versus 0 prone group. h/d (IQR, 0 to 0 h/d) in the control group.
By day 30 , 70 of 205 patients (34.1%) in the prone group were intubated versus 79 of 195 patients (40.5%) in the control group (hazard ratio, 0.81 [CI 95%, 0.59 to 1.12], P = 0.000). twenty; absolute difference, −6.37% [95% CI, −15.83% to 3.10%]).
Prone positioning did not significantly reduce 60-day mortality (hazard ratio, 0.93 [95% CI, 0.62 to 1.40], P = .54; absolute difference, -1.15% [95% CI, 0.62 to 1.40]. 95%, -9.40% to 7.10%]) and had no significant effect on days free from invasive mechanical ventilation or non-invasive ventilation at 30 days or on days free from the intensive care unit or the hospital at 60 days.
There were no serious adverse events in either group.
In the awake prone position group, 21 patients (10%) experienced adverse events, with the most frequently reported being musculoskeletal pain or discomfort from prone positioning (13 of 205 patients [6.34%]) and desaturation (2 of 205 patients [0.98%]).No adverse events were reported in the control group.
Conclusions and relevance
In patients with acute hypoxemic respiratory failure from COVID-19, prone positioning, compared with usual care without prone positioning, did not significantly reduce endotracheal intubation at 30 days.
However, the effect size for the study’s primary outcome was imprecise and does not exclude a clinically important benefit.















