A new study of nearly a quarter of a million asthma patients found that a high percentage have at least one coexisting type 2 (cT2) inflammatory disease, and patients with a higher inflammatory disease burden are more likely to experience asthma exacerbations. asthma.
Writing in the Journal of Asthma and Allergy , corresponding author David Price, MD, of the University of Aberdeen in Scotland, and colleagues explained that while asthma is a heterogeneous disease, the majority of asthma patients have type 2 asthma. , which is characterized by type 2 inflammation caused by cytokines such as interleukins 4 and 5.
Type 2 inflammation , driven by key cytokines including interleukins (IL)-4, -5, and -13, which are produced by T helper 2 cells and type 2 innate lymphoid cells, is a unifying feature of the allergic diseases and other classically defined inflammatory diseases. Approximately 50-70% of asthma patients have type 2 asthma, which is characterized by type 2 inflammation. The 2019 Global Initiative for Asthma (GINA) guidelines also highlight the type 2 phenotype among patients with severe asthma . Asthma is increasingly considered as part of a multimorbidity syndrome , and a large proportion of patients with asthma report symptoms of coexisting type 2 (cT2) inflammatory diseases such as eczema/atopic dermatitis, chronic rhinosinusitis with nasal polyposis, eosinophilia. esophagitis, allergic rhinitis or food allergies . Individual cT2 comorbidities may negatively impact patient quality of life and asthma-related outcomes. |
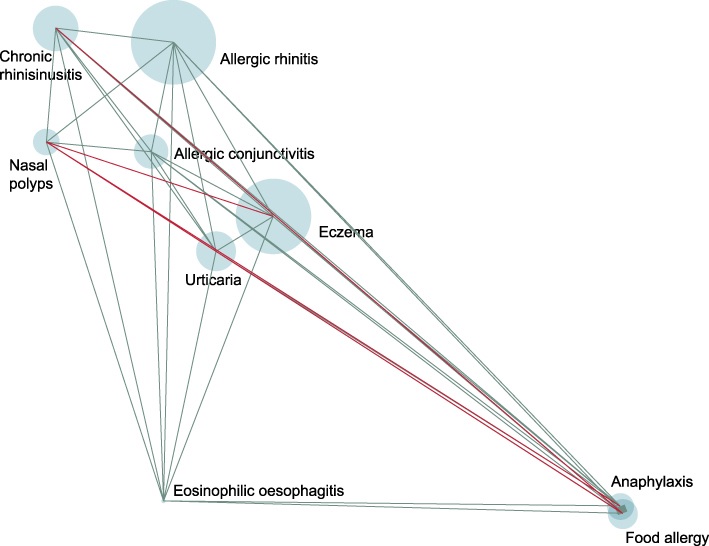
Clustering of medical service encounters related to type 2 inflammatory diseases among patients with asthma. The size of the circles is proportional to the prevalence of comorbidity. The width of the lines connecting the two comorbidities is proportional to the strength of their association. The color of the lines indicates the direction of the association: positive (teal) or negative (red). The position of comorbidities is based on rotated eigenvalues from principal component analyzes and shows proximity based on co-occurrence frequencies and strengths and directions of association.
“Asthma is increasingly considered to be part of a multimorbidity syndrome , and a large proportion of asthma patients report symptoms of cT2 inflammatory diseases, such as atopic eczema/dermatitis, chronic rhinosinusitis with nasal polyposis, eosinophilic esophagitis, allergic rhinitis, or allergies. food, Price and his colleagues wrote.
Reports have been published highlighting the prevalence of cT2 inflammatory diseases among patients with asthma, but these reports have been based on patients’ self-reports rather than medical service encounters and diagnoses, the authors said.
In the new report, researchers used real-world data to calculate cT2 rates and the impact of those comorbidities in asthma patients. They used an original data set of medical records from 4.5 million patients from 650 primary care practices in the United Kingdom between 2010 and 2017.
Patients were included if they had at least 1 diagnosis code for asthma and at least 2 asthma-related prescriptions in the year before the index date. Patients were assigned a cT2 burden score (ranging from 0 to 9) based on the total number of coexisting diseases with which they had been diagnosed.
After exclusions for factors such as chronic lower respiratory diseases, including chronic obstructive pulmonary disorder (COPD), the researchers were left with a total of 245,893 asthma patients. The mean (SD) age of the group was 44.8 years (22.1) and 43.8% were men.
The authors found that 55% of patients with Global Initiative for Asthma (GINA) step 1 asthma (the least severe) had a medical diagnosis of at least one other type 2 inflammatory disease . Among patients with GINA grade 5 asthma (the highest step on the scale), 60% had at least one other type 2 inflammatory disease diagnosis.
Additionally, the researchers found that the higher the cT2 burden score, the more likely a patient was to experience asthma exacerbations and the less likely they were to achieve asthma control.
Price and colleagues said they believe theirs is the first study to show how multiple cT2s, beyond allergic rhinitis, can affect asthma control. They said their findings align with previous research suggesting that patients with cT2 are more likely to experience exacerbations.
They concluded that their findings should prompt doctors to reconsider the risk profile of patients with asthma and other inflammatory diseases.
"As the presence of cT2 complicates asthma treatment and is associated with an increased risk of exacerbations and poorer asthma control, clinicians may consider assessing the burden of type 2 comorbidity in their evaluation of patients with moderate to moderate asthma. serious," he wrote.
Discussion
Type 2 asthma is a widely prevalent type of persistent and uncontrolled asthma26 and includes allergic asthma and eosinophilic asthma phenotypes, which have overlapping pathophysiological mechanisms.8 It is well established that IL-4 and IL-13 are key drivers of cT2, such as atopic dermatitis, allergic rhinitis, nasal polyps and eosinophilic esophagitis related to cT2 among patients with asthma.
Although the impact of cT2, such as allergic rhinitis, on healthcare resource utilization among patients with asthma has been previously investigated, to our knowledge, few studies have investigated the impact of global cT2 burden on asthma exacerbations and asthma control.
A cross-sectional observational study found that coexisting allergic rhinitis was associated with an incremental adverse impact on the level of asthma control; Meanwhile, a second cross-sectional observational study found that patients who reported severe rhinitis had worse asthma control than those with mild or no rhinitis symptoms.
The trends observed in these two cross-sectional studies are reflected in our study as asthma patients with higher cT2 had poorer asthma control compared to asthma patients with lower cT2. However, we believe that our study is the first to reveal the impact of multiple cT2 on asthma control, beyond allergic rhinitis.
The results of this study also confirm that asthma patients with cT2 were at increased risk of severe exacerbations compared to asthma patients with less cT2, which is supported by previously published evidence demonstrating the association between asthma and Comorbid allergic rhinitis and increased exacerbations.
Among patients with asthma, cT2 burden first peaked among the 5- to 9-year-old and 10- to 19-year-old cohorts, and then appeared to decline in the older age groups. This trend is not unusual, as it is understood that some children may outgrow cT2 such as eczema and food allergies . The burden of type 2 comorbidities was high across all GINA steps, and most patients with asthma had a diagnosis of at least one other cT2
Conclusions This real-world retrospective database study has shown that patients with asthma received cT2-related medical services, which increased resource use among patients with asthma. The presence of type 2 comorbidities is associated with a higher risk of exacerbations and poorer asthma control. Because the presence of cT2 complicates asthma treatment and is associated with an increased risk of exacerbations and poorer asthma control, clinicians may consider assessing type 2 comorbidity burden in their evaluation of patients with moderate to severe asthma. . |
Reference:
Price D, Menzies-Gow A, Bachert C, et al. Association between a type 2 inflammatory disease burden score and outcomes in patients with asthma. J Asthma allergy. Published online September 29, 2021. doi:10.2147/JAA.S321212















