Key points What are the epidemiological trends and prognostic factors of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in patients in the US? Findings In this cohort study of 43,751 patients with GEP-NETs, most cases occurred in the rectum and small intestine. The age-adjusted incidence rate of GEP-NETs increased significantly from 1975 to 2015, especially for grade 1, localized, and rectal GEP-NETs; Age, sex, marital status, and tumor size, grade, stage, and site were significantly associated with the overall survival of GEP-NET patients. Meaning The incidence and prevalence of GEP-NETs have continued to increase for 40 years; This study suggests that a predictive model based on prognostic factors can accurately quantify the risk of death among patients with GEP-NETs, indicating that the model has satisfactory clinical practicality. |
Neuroendocrine tumors (NETs) are a heterogeneous class of rare cancers with different biological behaviors arising from cells throughout the diffuse endocrine system. Because approximately two-thirds of NETs occur in the gastroenteropancreatic system, which primarily includes the stomach, small intestine, colon, appendix, rectum, and pancreas, gastroenteropancreatic NETs (GEP-NETs) are the major subtype of TNE.
The biological behavior of some tumors is relatively indolent, other GEP-NETs may be more aggressive and be associated with a poor prognosis.
The increasing number of articles published each year on NETs demonstrates that global attention to NETs has increased, which could be due to the increase in reported incidence. However, to the best of our knowledge, there is a lack of updated data on epidemiological characteristics. and in the survival analysis of patients with GEP-NET.
On the other hand, given the rarity and indolent biological behavior of GEP-NETs, most studies on GEP-NETs are based on a small (or very small) number of cases at individual institutions.
Based studies have never specifically targeted GEP-NETs, but have only addressed the problem of NETs at a single site in the gastrointestinal tract (e.g., stomach, colon, small intestine, appendix, or pancreas). ). Therefore, in this study, we conducted a population-based study using information from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute to systematically analyze the epidemiological, clinical, and prognostic characteristics of GEP-NETs.
Due to the complex and inconsistent treatment of GEP-NETs, the prognosis of patients with GEP-NETs remains difficult to evaluate. To date, prognostic analysis of NETs is still mainly based on the American Joint Committee on Cancer and the European Neuroendocrine Oncology TNM staging system. This system evaluates the prognosis of patients based on tumor volume (T), tumor involvement of regional lymph nodes (N), and distant metastases (M).
However, other basic clinicopathologic characteristics, such as age, sex, race and ethnicity, and tumor grade and location, may also be associated with patients’ prognosis. Among the prediction tools currently available, nomograms are considered the most accurate and characteristic method. to predict the prognosis of cancer patients.
For certain malignancies, patient mortality risk has been successfully quantified by combining relevant prognostic factors. However, to our knowledge, few studies have used nomograms to predict the prognosis of patients with GEP-NET.
This study sought to develop a more detailed nomogram based on the relatively large cohort of GEP-NET patients in the SEER database to predict 3- and 5-year overall survival (OS).
Importance
Although the incidence and prevalence of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) are believed to have increased over the past decades, updated epidemiological and survival data are lacking.
Goals
To perform an epidemiological and survival analysis of the largest cohort of GEP-NET patients using the most recent data and establish a new nomogram to predict the survival probability of individual GEP-NET patients.
Design, environment and participants
In this cohort study, 43,751 GEP-NET patients diagnosed from January 1, 1975 to December 31, 2015 were identified from the Surveillance, Epidemiology, and End Results Program.
The associated data were used for epidemiological and survival analysis, as well as for the establishment and validation of a nomogram to predict the probability of survival of individual patients with GEP-NETs.
The cut-off date of the study was December 31, 2018. The statistical analysis was carried out from February 1 to April 30, 2020.
Main results and measures
Incidence, factors associated with overall survival, and a nomogram model for patients with GEP-NETs.
Results
A total of 43,751 patients were diagnosed with GEP-NET between 1975 and 2015 (22,398 women [51.2%], 31,976 white patients [73.1%], 7,097 black patients [16.2%], 3,207 Asian patients, and Pacific Islanders [7.3%], 270 American Indian and Alaska Native patients [0.6%], and 4,546 patients of unknown race [10.4%]; mean [SD] age at diagnosis, 58 [ 15 years).
The age-adjusted incidence rate of GEP-NETs increased 6.4-fold between 1975 and 2015 (annual percentage change [ACP], 4.98; 95% CI, 4.75 to 5.20; P < 0.001) . Furthermore, among the site groups, the incidence of GEP-NET in the rectum increased more significantly (APC, 6.43; 95% CI, 5.65-7.23; P < 0.001).
Regarding stage and grade, the incidence increased more in localized GEP-NETs (APC, 6.53; 95% CI, 6.08-6.97; p <0.001) and G1 GEP-NETs (CPA, 18.93; 95% CI, 17.44-20.43; p <0.001).
During the study period, the mean age at diagnosis of localized disease increased by 9.0 years (95% CI, 3.3-14.7 years; P = 0.002), which remained unchanged for regional and remote cases.
In multivariable analyses, age, sex, marital status, and tumor size, grade, stage, and site were significantly associated with overall survival of patients with GEP-NETs (e.g., patients with distant versus localized disease: hazard ratio, 10.32; 95% CI, 8.56-12.43; G4 vs G1 GEP-NET: hazard ratio, 6.37; 95% CI, 5.39-7.53).
Additionally, a nomogram comprising age, size, grade, stage, and site was established to predict the probability of 3- and 5-year survival, with concordance rates of 0.893 (95% CI, 0.883-0.903) for internal validations and 0.880 (95% CI, 0.866-0.894) for external validations.
The receiver operating characteristic curve demonstrated that the nomogram exhibited better discriminatory power than the TNM classification (area under the curve for 3-year overall survival, 0.908 vs. 0.795; for 5-year overall survival, 0.893 vs. 0.791).
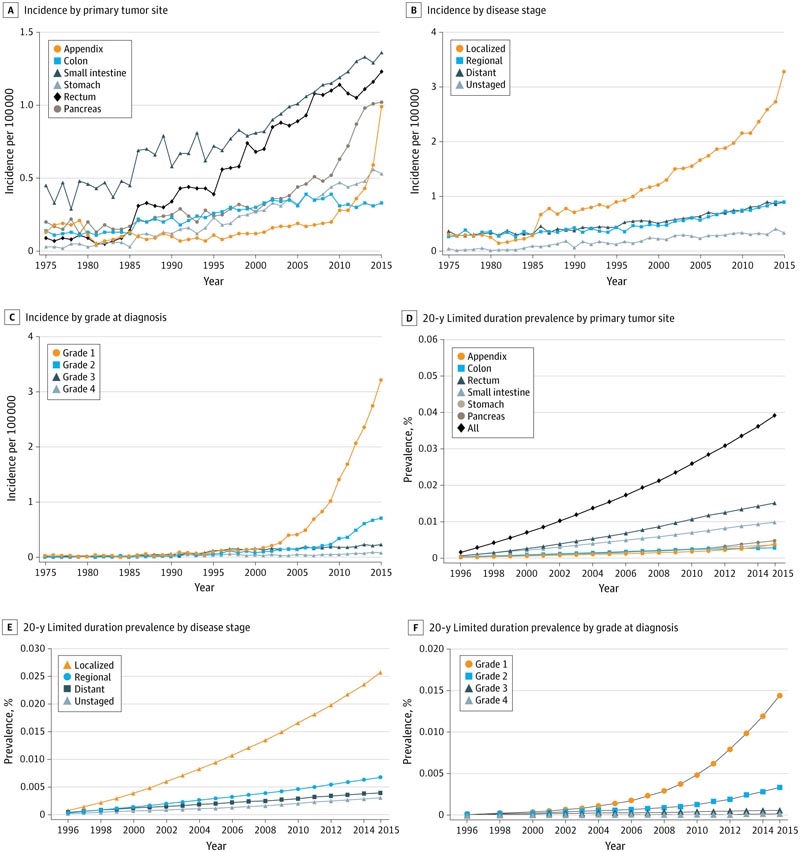
Incidence and Time-Limited Prevalence of Gastroenteropancreatic Neuroendocrine Tumors (GEP-NETs) Over Time by Site, Disease Stage, and Grade
Conclusions and relevance
In this study, the incidence and prevalence of GEP-NETs has continued to increase for 40 years, especially among patients with rectal GEP-NETs. Furthermore, this study suggests that a nomogram with 5 prognostic parameters can accurately quantify the risk of death among GEP-NET patients, indicating that it has satisfactory clinical practicality.
Comments
Gastroenteropancreatic (GEP) neuroendocrine tumors (NETs) are a heterogeneous and rare group of diseases with a natural history ranging from indolent to very aggressive.
There is evidence of a higher incidence of these tumors in recent retrospective series. Researchers now report a cohort study evaluating epidemiological and survival data in nearly 44,000 patients with GEP NETs from 1975 to 2015 from the US Surveillance, Epidemiology, and End Results (SEER) Program.
Incidence was similar in men and women, and age-adjusted incidence rates increased over time. Rates increased similarly across all races and some ethnicities, but were most stable in Alaska Natives and American Indians.
Increase rates were highest for localized and grade 1 NETs, with rectal and small bowel tumors having the highest prevalence. The mean age at diagnosis of localized disease increased by 9 years during the study period.
The median overall survival (OS) was as follows:
|
This large series supports the observation of a higher incidence of GEP NETs. An increase in diagnosis may result from the increasing use of cross-sectional imaging, and overall survival may continue to improve with the advent of more effective systemic and regional therapies.
Conclusions and final message
In this study, the incidence and prevalence of GEP-NETs has continued to increase for 40 years, especially in specific sites (such as the rectum and stomach). Differences in survival rates were observed based on primary tumor site, tumor grade, and tumor stage. However, as diagnosis and treatment progressed, outcomes generally improved.
Furthermore, a new nomogram, in which tumor stage was the most useful factor, established and validated in the present study, can effectively predict the 3- and 5-year survival rates of GEP-NET patients. It could provide doctors and patients with accurate and useful information and guide the treatment strategy for patients with GEP-NETs.
















