Colorectal cancer (CRC) is the third leading cause of cancer death in the United States. Screening has been shown to decrease CRC incidence and mortality by identifying and eliminating precancerous polyps and early cancers. Among the screening options available, colonoscopy is the most widely used in the United States.
Despite the overall increase in uptake of CRC screening, a substantial disparity in uptake remains, with approximately 40% of screening-eligible American adults not meeting recommendations.
These data highlight the importance of adapting screening recommendations based on the risk profile to optimize the benefit of screening and resource allocation at the population level.
Currently, CRC screening is recommended only based on age and family history. Although several studies have examined CRC risk prediction based on clinical, lifestyle, environmental, and genetic factors, those studies aimed to develop screening recommendations based on predicted CRC risk or examined the joint effect of predictors and CRC risk screening. To our knowledge, no previous study has directly examined whether the benefit of screening differs by risk profile.
The optimal age to initiate screening is a critical component of screening recommendations. Since 2002, the US Preventive Services Task Force (USPSTF) has recommended that CRC screening begin at age 50 in average-risk adults.
Given the increasing incidence of early-onset CRC in recent years, in 2020, the USPSTF published the draft recommendation that average-risk adults can begin routine screening at age 45 instead of 50. The American Society of Cancer has made a similar recommendation. These recommendations for earlier screening have sparked intense debate about the risk-benefit ratio and have led to increased interest in the development of risk-based screening strategies.
Therefore, in the present study, we prospectively assessed the relative and absolute risk of CRC incidence and mortality associated with colonoscopy screening based on the risk profiles of individuals within 2 large US cohorts, including the Nurses’ Health Study. (NHS) and the Health Professionals Follow-up Study (HPFS). We also examined the cumulative incidence of CRC by age and identified the ages at which the CRC risk threshold was reached at 45 and 50 years, respectively, among individuals with different CRC risk profiles.
Background It is unknown whether the benefit of colonoscopy screening for colorectal cancer (CRC) and the optimal age to start screening differ by CRC risk profile. Methods Among 75,873 women and 42,875 men, a CRC risk score (0-8) was defined based on family history, aspirin, height, body mass index, smoking, physical activity, alcohol, and the diet. Hazard ratios associated with colonoscopy screening and absolute risk reductions (ARRs) were calculated for CRC incidence, mortality, and cumulative CRC incidence by age based on risk score. All statistical tests were two-sided. Results During a median of 26 years of follow-up , 2407 CRC cases and 874 CRC deaths were documented. Although the hazard ratio associated with screening did not vary as a function of risk score, the variable-adjusted hazard ratio for 10-year CRC incidence was more than double for individuals with scores of 6 to 8 (hazard ratio risk = 0.34%, 95% confidence interval [CI] = 0.26% to 0.42%) compared with 0-2 (hazard ratio = 0.15%, 95% CI = 0. 12% to 0.18%, trend < 0.001). Similar results were found for CRC mortality (ARR = 0.22%, 95% CI = 0.21% to 0.24% vs. 0.08%, 95% CI = 0.07% to 0. 08%, Ptrend < 0.001). The ARR for mortality from distal colon and rectal cancers was four times higher for scores 6-8 than for scores 0-2 (distal colon cancer: ARR = 0.08%, 95% CI = 0.07 % to 0.08% vs 0.02%, 95% CI = 0.02% to 0.02%, Ptrend < 0.001; rectal cancer: ARR = 0.08%, 95% CI = 0.08 % to 0.09% vs 0.02%, 95% CI = 0.02% to 0.03%, Ptrend < .001). When age 45 years was used as the baseline to start screening, individuals with risk scores of 0-2, 3, 4, 5, and 6-8 reached the CRC risk level (10-year cumulative risk). 0.47%) at the age of 51 years, 48 years, 45 years, 42 years and 38 years, respectively. Conclusions The absolute benefit of colonoscopy screening is more than double for individuals with the highest rather than the lowest CRC risk profile. Individuals with a high- and low-risk profile can begin screening up to 6-7 years before and after, respectively, the recommended age of 45 years. |
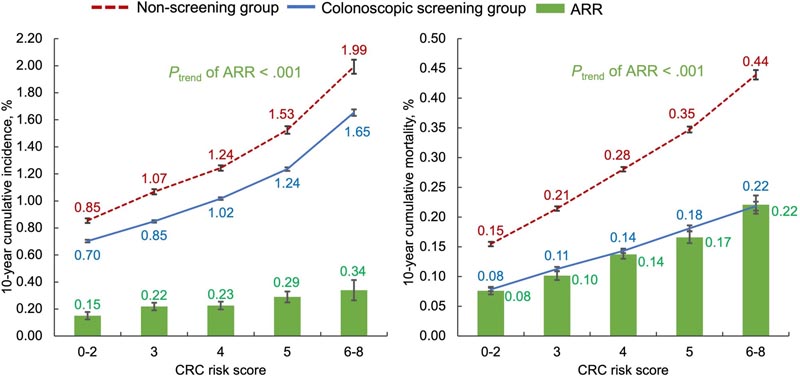
Variable-adjusted 10-year cumulative incidence (left panel) and mortality (right panel) of colorectal cancer (CRC) and corresponding absolute risk reduction (ARR) by CRC risk score. CRC risk score (range = 0-8) was defined as the number of 8 high CRC risk factors: having a family history of CRC among first-degree relatives, not regularly using aspirin (<2 tablets or times per week), tall stature (higher 50% of height in each cohort), overweight or obese (body mass index ≥25.0 kg/m2), current or former smoker with 5 or more pack-years, low physical activity (<30 min/d of moderate to vigorous intensity activity), excessive alcohol consumption (≥1 drink [14 g of alcohol] per day for women and ≥2 drinks per day for men), and unhealthy diet ( that meets <3 of the 6 dietary recommendations of the 2018 World Cancer Research Fund/American Institute for Cancer Research Report, which included red meat <0.5 serving per day, processed meat <0.2 serving per day, dietary fiber ≥30 g/d, dairy products ≥3 servings per day, whole grains ≥48 g/d representing at least half of the total grains, and use of calcium supplements). We examined the trend of ARRs across CRC risk scores by regressing multivariable-adjusted cumulative risk on baseline colonoscopy screening status and CRC risk score, as well as their product term, whose P value was derived as the Ptrend. The tests were two-sided. Error bars indicate 95% confidence intervals.
Comments
Age and family history inform recommendations for colorectal cancer (CRC) screening, but other risk factors have been identified.
In this study, researchers used two long-term US cohort studies - the Nurses’ Health Study and the Health Professionals Follow-Up Study - to examine 8 risk factors known to be associated with an excess incidence of CRC: family history, smoking, higher body mass index, less physical activity, unhealthy diet, alcohol consumption, tall stature, and lack of aspirin use (specific definitions of each risk factor are detailed in an online supplement published with the original article). About 120,000 participants (mean age, 54 years) were followed for an average of 26 years.
Adjusted analyzes revealed the following
- The 10-year risk of developing CRC in low-risk participants (0-2 risk factors) was 0.85% in those who had not undergone a screening colonoscopy and 0.70% among those who did. They had submitted to it. On the other hand, in high-risk people (6-8 risk factors), these percentages were 1.99% and 1.65%, respectively.
- CRC-related 10-year mortality in low-risk participants (0-2 risk factors) was 0.15% without screening colonoscopy and 0.08% with it. On the other hand, in high-risk people (6-8 risk factors), these percentages were 0.44% and 0.22%, respectively.
These risk factors - combined into an 8-point score - predicted two-fold differences in CRC incidence and three-fold differences in CRC-related mortality.
Current guidelines recommend screening based on age alone (with earlier screening in people with CRC in first-degree relatives), and the guidelines are unlikely to incorporate more refined risk scores in the foreseeable future.
However, for patients who are reluctant to undergo screening, clinicians could use such scores to promote more informed decision-making. One caveat: Almost all participants in this study were white healthcare professionals.
| In conclusion , the absolute benefits of colonoscopy screening for the prevention of CRC and related death are more than double for individuals with the highest rather than the lowest CRC risk profile. Individuals with a high and low CRC risk profile can begin CRC screening up to 6-7 years before and after, respectively, the recommended age of 45 or 50 years. Our data support the importance of risk-based screening recommendations. |
















