Key points How often do diagnostic errors occur in adult patients who are transferred to the intensive care unit (ICU) or die in the hospital, what causes the errors, and what are the associated harms? Findings In this cohort study of 2428 patient records, a missed or delayed diagnosis occurred in 23%, and 17% of these errors caused temporary or permanent harm to patients. The underlying problems in the diagnostic process with the largest effect sizes associated with diagnostic errors, and which could be an initial focus for safety improvement efforts, were failures in testing and clinical evaluation. Meaning Among hospitalized adults transferred to the ICU or who died in hospital, diagnostic errors were common, harmful, and had underlying causes, which can be used to design future interventions. |
Importance
Diagnostic errors contribute to patient harm, although few data exist to describe their prevalence or underlying causes among hospitalized medical patients.
Aim
To determine the prevalence, underlying cause, and harms of diagnostic errors among hospitalized adults transferred to an intensive care unit (ICU) or who died.
Design, environment and participants
Retrospective cohort study conducted at 29 US academic medical centers in a random sample of adults hospitalized with general medical conditions and who were transferred to an ICU, died, or both between January 1 and December 31, 2019 .
Each record was reviewed by two trained clinicians to determine whether a diagnostic error occurred (i.e., missed or delayed diagnosis), identify flaws in the diagnostic process, and classify harms.
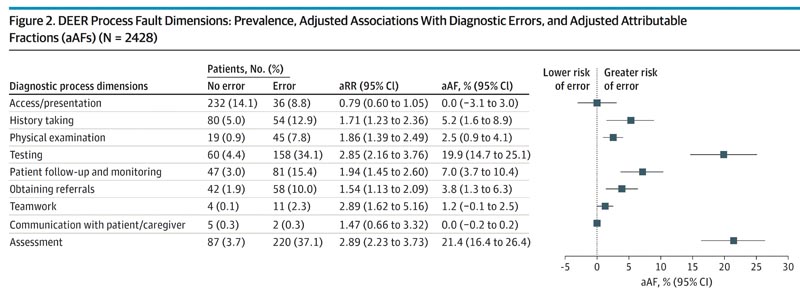
Multivariable models estimated the association between process failures and diagnostic errors. The opportunity for reduction in diagnostic errors associated with each failure was estimated using the adjusted proportion attributable fraction (aPAF). Data analysis was carried out from April to September 2023.
Main results and measures
Whether or not a diagnostic error occurred, the frequency of the underlying causes of the errors, and the harms associated with those errors.
Results
Of 2428 patient records at 29 hospitals that underwent review (mean [SD] patient age, 63.9 [17.0] years; 1107 [45.6%] women and 1321 [54.4%] men) , 550 patients (23.0%; 95% CI (20.9%-25.3%) had experienced a diagnostic error.
Errors were considered to have contributed to temporary harm, permanent harm, or death in 436 patients (17.8%; 95% CI, 15.9%-19.8%); among the 1,863 patients who died, diagnostic error was considered to have contributed to death in 121 (6.6%; 95% CI, 5.3%-8.2%).
In multivariable models examining process failures associated with any diagnostic error, patient assessment problems (aPAF, 21.4%; 95% CI, 16.4%-26.4%), and problems with ordering and interpretation of tests (aPAF, 19.9%; 95% CI, 14.7%). -25.1%) had the greatest opportunity to reduce diagnostic errors; Similar classification was observed in multivariable models examining harmful diagnostic errors.
Conclusions and relevance In this cohort study, diagnostic errors in hospitalized adults who died or were transferred to the ICU were common and associated with patient harm. Problems with the choice and interpretation of tests and the processes involved with medical evaluation are high priority areas for improvement efforts. |















