Summary Background Recent single-center reports have suggested that community-acquired bacteremic coinfection in the context of coronavirus disease 2019 (COVID-19) may be an important factor in mortality; however, these reports have not been validated with a multicenter, demographically diverse cohort study with data spanning the pandemic. Methods In this multicenter retrospective cohort study, inpatient encounters for COVID-19 with community-acquired bacteremic coinfection were evaluated using 48-hour post-admission blood cultures and grouped by: (1) confirmed coinfection [recovery of bacterial pathogen ], (2) suspected coinfection [culture negative with ≥2 antimicrobials administered], and (3) no evidence of coinfection [no culture]. The primary outcomes were in-hospital mortality, ICU admission, and mechanical ventilation. Risk factors for COVID-19 bacterial coinfection and impact on primary outcomes were determined using multivariate logistic regressions and expressed as adjusted odds ratios with 95% confidence intervals (cohort, OR 95% CI, p of the Wald test). Results Cohorts studied included 13,781 inpatient encounters with COVID-19 between 2020 and 2022 at the University of Alabama at Birmingham (UAB, n = 4,075) and Ochsner Louisiana State University Health—Shreveport (OLHS, n = 9,706) with confirmed cohorts (2.5%), suspected (46%), or no community-acquired bacterial coinfection (51.5%), and a comparison cohort consisting of 99,170 inpatient encounters between 2010 and 2019 (UAB Prepandemic Cohort before COVID-19). A significantly higher likelihood of COVID-19 bacterial co-infection was observed in patients with a high neutrophil-to-lymphocyte ratio ≥ 15 (UAB: 1.95 [1.21–3.07]; OLHS: 3.65 [2.66 –5.05], p < 0.001 for both) within 48 hours of hospital admission. Bacterial co-infection was found to confer the greatest increased risk of in-hospital mortality (UAB: 3.07 [2.42–5.46]; OLHS: 4.05 [2.29–6.97], p < 0.001 for both ), ICU admission (UAB: 4.47 [ 2.87–7.09], OLHS: 2.65 [2.00–3.48], p < 0.001 for both) and mechanical ventilation (UAB: 3, 84 [2.21–6.12]; OLHS: 2.75 [1.87–3.92], p < 0.001 for both) in both cohorts, compared with other risk factors for severe disease. The mortality observed in COVID-19 bacterial coinfection (24%) dramatically exceeds the mortality rate associated with community-acquired bacteremia in patients hospitalized before the COVID-19 pandemic (5.9%) and was consistent in alpha, delta and omicron SARS-CoV -2 variants. Conclusions Elevated neutrophil to lymphocyte ratio is a prognostic indicator of COVID-19 bacterial co-infection within 48 hours of admission. Community-acquired bacterial co-infection, defined by positive blood culture results, confers a higher risk of in-hospital mortality, ICU admission, and mechanical ventilation than previously described risk factors (advanced age, selected comorbidities, male sex) for COVID-19. mortality, and is independent of the SARS-CoV-2 variant. |
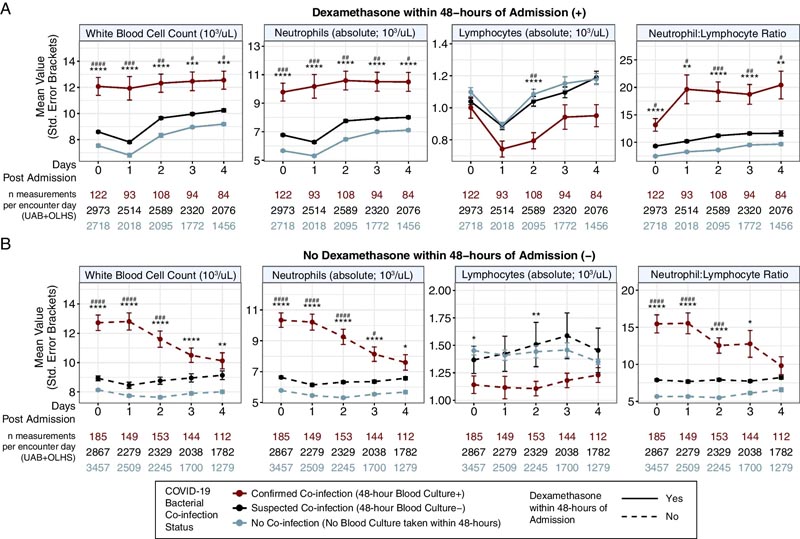
The elevated neutrophil to lymphocyte ratio (≥ 15) in patients with COVID-19 bacterial coinfection is independent of dexamethasone treatment within 48 hours of hospital admission. Post-admission laboratory trends for inpatient COVID-19 encounters pooled from the UAB and OLHS cohorts and stratified by confirmed, suspected, and no coinfection bacterial coinfection and 48-hour dexamethasone treatment. Mean laboratory values with standard error bars from the day of admission (day 0) to 4 days post-admission are shown for patients A with dexamethasone treatment within 48 h (solid lines) and B without dexamethasone treatment within 48 h (dashed line) , all stratified by COVID-19 co-infection status. Statistical significance was assessed using Bonferroni corrected t tests: (p < 0.0001 = ****/####, p < 0.001 = ***/###, p < 0.01 = **/ ##, p < 0.05 = */#). Reference group (red): Coinfection confirmed 48 h after admission blood culture (+). Comparison group 1 (light blue, *): No coinfection. Comparison group 2 (dark blue; #): Suspected coinfection 48 h after blood culture admission (-). UAB, University of Alabama at Birmingham cohort; OLHS, Ochsner Louisiana State University Health—Shreveport Cohort
Comments
Having a bacterial infection at the same time as COVID-19 is a greater risk factor for COVID-19 severity and mortality than the risk factors described above, such as older age, male sex, or various comorbidities.
Bacterial coinfection is a significant risk factor for death, intensive care unit admission, and mechanical ventilation, according to a multicenter retrospective cohort study published in the journal Critical Care and led by researchers at the University of Alabama at Birmingham.
Coronavirus disease 2019, or COVID-19, has killed more than 6.3 million people worldwide.
This recent study of 13,781 hospitalized COVID-19 patient encounters from 2020 to 2022 found that bacterial co-infection in the blood, known as bacteremia, is a major risk factor for death, intensive care unit admission, and mechanical ventilation than the risk factors described above for COVID -19 severity and mortality, such as older age, male sex, or various comorbidities.
The study reviewed inpatient encounters with COVID-19 at UAB Hospital and Ochsner Louisiana State University Health Shreveport hospitals and divided them into three groups: Confirmed bacterial coinfection, as measured by a blood test 48 hours later of admission; suspected bacterial coinfection in patients receiving antimicrobials; and no bacterial coinfection.
Bacterial co-infection is a known major source of illness and death in the context of other respiratory viral infections such as influenza, parainfluenza or RSV. However, it has remained unclear regarding the frequency of bacteremic co-infection in COVID-19 and the impact it has on clinical outcomes.
"Although confirmed bacteremic co-infections are rare in COVID-19, less than 4 percent of inpatient admissions, our results show that COVID-19 patients with these co-infections have a staggering 25 percent risk of death at 30 days in UAB patients and a similar 20 percent risk at Ochsner Louisiana State University Health Shreveport, or OLHS,” said Amit Gaggar, M.D., Ph.D., Division of Pulmonary, Allergy and Critical Care Medicine, Department of Medicine. the UAB. Gaggar, in collaboration with Precision Medicine Institute Director Hugh Kaul, Matthew Might, Ph.D., and infectious diseases physician and scientist Nathaniel Erdmann, M.D., Ph.D., co-led the study.
“These results strongly suggest an underestimated interaction between bacterial pathogens and the COVID-19 virus, SARS-CoV-2, and its impact on clinical outcomes,” added co-senior author Erdmann.
Specifically, the researchers found that in-hospital mortality from COVID-19 coinfections of 26 percent at UAB and 22 percent at OLHS exceeded that of suspected coinfection (UAB, 24 percent; OLHS, 12 percent) and not coinfection groups (UAB, 5.9 percent; OLHS, 5.1 percent). Additionally, a control group of 1,703 patients hospitalized at UAB with community-acquired bacteremia during a period before the COVID-19 pandemic had an in-hospital mortality rate of 5.9 percent.
The researchers also identified laboratory trends associated with COVID-19 bacterial coinfection: a neutrophil-to-lymphocyte ratio of 15 or higher, and Systemic Inflammatory Response Syndrome, or SIRS, criteria for abnormal white blood cell counts or a heart rate. greater than 90 beats per minute. These can help healthcare providers discriminate against COVID-19 bacterial co-infections within 24 hours of admission.
"These results emphasize the role of bacteria in SARS-CoV-2 mortality and highlight the potential of the neutrophil-to-lymphocyte ratio as a rapid and readily available prognostic biomarker of bacterial co-infection and, relatedly, the severity of the disease," said the co-director.
The strengths of this study were the two large, independent, demographically diverse cohorts: the UAB reflects an academic hospital and Level I trauma center serving five surrounding states, and the OLHS includes gatherings of rural, suburban, and academic medical centers in the entire state of Louisiana. Both cohorts were generally well matched for patients’ age, race, sex, and length of hospitalization.
“One of the new opportunities of the COVID-19 pandemic has been the seismic shift in the collected and searchable data captured by electronic medical record, or EMR, systems. “This resource, combined with the collaborative spirit of UAB and OLHS experts, provides the foundation for biomedical informatics studies that can produce clinically useful observations for patient improvement,” said the study’s lead and corresponding author. , Michael John Patton.
Final message This retrospective multicenter analysis identified COVID-19 bacterial coinfections in independent cohorts using 48-h blood culture results. Our analysis confirmed elevated levels of NLR ≥ 15 and SIRS criteria components were early and unequivocal biomarkers of COVID-19 bacterial co-infections. We evaluated the clinical impact of COVID-19 co-infection and found a higher likelihood of ICU admission, mechanical ventilation, and in-hospital mortality compared to COVID-19 infection alone that was independent of the SARS-CoV-2 variant (p (e.g., alpha, delta, omicron). Finally, we show that COVID-19 bacteraemic co-infection has a five-fold higher in-hospital mortality rate compared to patients hospitalized before the COVID-19 pandemic with bacteremia within 48 hours of admission. |