Atrial fibrillation is a heterogeneous disorder with a variable course. About one-third of atrial fibrillation cases that begin as brief paroxysmal episodes that end on their own progress to longer-lasting persistent attacks over time. Once the transition from paroxysmal to persistent atrial fibrillation occurs, the likelihood of treatment success decreases and the risks of adverse clinical outcomes increase. Therefore, treatment strategies are needed to prevent progression to persistent forms of atrial fibrillation. However, what strategies are successful and how soon should we intervene?
Background
Atrial fibrillation is a chronic, progressive disorder, and persistent forms of atrial fibrillation are associated with increased risks of thromboembolism and heart failure. Catheter ablation as initial therapy may modify the pathogenic mechanism of atrial fibrillation and alter the progression to persistent atrial fibrillation.
Methods
We report the 3-year follow -up of patients with untreated paroxysmal atrial fibrillation who were enrolled in a trial in which they had been randomly assigned to undergo initial rhythm control therapy with cryoballoon ablation or to receive antiarrhythmic drug therapy.
All patients had implantable loop recorders fitted at the time of trial entry, and evaluation was performed using downloaded daily logs and in-person visits every 6 months.
Data on first episode of persistent atrial fibrillation (lasting ≥7 days or lasting 48 hours to 7 days but requiring cardioversion to terminate), recurrent atrial tachyarrhythmia (defined as atrial fibrillation, flutter, or tachycardia lasting ≥30 seconds), the burden of atrial fibrillation (percentage of time in atrial fibrillation), quality of life metrics, healthcare utilization,
Results
A total of 303 patients were enrolled , with 154 patients assigned to receive initial rhythm control therapy with cryoballoon ablation and 149 assigned to receive antiarrhythmic drug therapy.
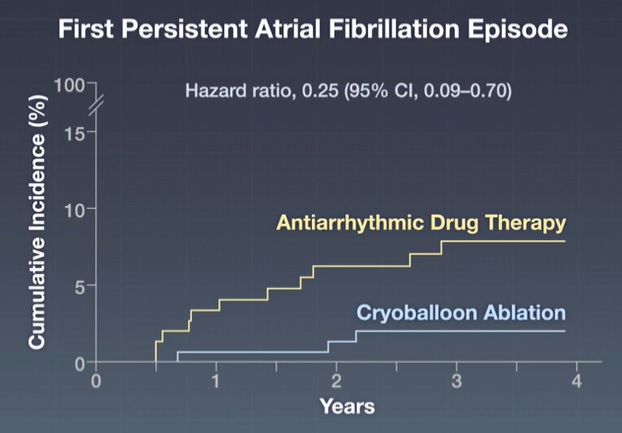
During 36 months of follow-up, 3 patients (1.9%) in the ablation group had an episode of persistent atrial fibrillation, compared with 11 patients (7.4%) in the antiarrhythmic drug group (hazard ratio, 0 .25; 95% confidence interval). [CI], 0.09 to 0.70).
Recurrent atrial tachyarrhythmia occurred in 87 patients in the ablation group (56.5%) and 115 in the antiarrhythmic drug group (77.2%) (hazard ratio, 0.51; 95% CI, 0.38). to 0.67).
The median percentage of time in atrial fibrillation was 0.00% (interquartile range, 0.00 to 0.12) in the ablation group and 0.24% (interquartile range, 0.01 to 0.94) in the ablation group. in the group of antiarrhythmic drugs.
At 3 years , 8 patients (5.2%) in the ablation group and 25 (16.8%) in the antiarrhythmic drug group had been hospitalized (relative risk, 0.31; 95% CI, 0. 14 to 0.66).
Serious adverse events occurred in 7 patients (4.5%) in the ablation group and 15 (10.1%) in the antiarrhythmic drug group.
Conclusions Initial treatment of paroxysmal atrial fibrillation with catheter cryoballoon ablation was associated with a lower incidence of persistent atrial fibrillation or recurrent atrial tachyarrhythmia over 3 years of follow-up than initial use of antiarrhythmic drugs. |
(Funded by Cardiac Arrhythmia Network of Canada and others; EARLY-AF ClinicalTrials.gov number, NCT02825979. opens in new tab.)















