Starting in December 2019, a cluster of pneumonia cases with unknown cause was reported in Wuhan, Hubei province of China. On January 7, 2020, a new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; formerly known as 2019-nCoV), was identified as the causative organism.
SARS-CoV-2 has been shown to infect human respiratory epithelial cells through an interaction between the viral S protein and the angiotensin-converting enzyme receptor on human cells; Thus, SARS-CoV-2 has a strong capacity to infect humans.
The clinical characteristics of the initial 41 patients confirmed as infected with SARS-CoV-2 included lower respiratory tract disease with fever, dry cough and dyspnea, a manifestation similar to those of two other diseases caused by coronavirus, severe acute respiratory syndrome (SARS). ) and Middle East respiratory syndrome (MERS). However, radiological changes in the lungs of people with COVID-19 pneumonia have not been fully characterized.
CT is important in the diagnosis and treatment of lung diseases.
Imaging features of COVID-19 pneumonia are diverse, ranging from normal appearance to diffuse changes in the lungs. Furthermore, different radiological patterns are observed at different times throughout the course of the disease.
Because the time between the onset of symptoms and the development of acute respiratory distress syndrome (ARDS) was short among initial patients with COVID-19 pneumonia, early recognition of the disease is essential for the treatment of these patients. .
The objective was to analyze the evolution of chest CT imaging features in patients with COVID-19 pneumonia, and compare imaging findings throughout the course of the disease, to facilitate early diagnosis of this emerging and potentially mortal.
Methods
Patients with COVID-19 pneumonia who were admitted to one of the two hospitals in Wuhan and who underwent serial chest CT scans were retrospectively included. Patients were grouped according to the interval between the onset of symptoms and the first CT:
- Group 1 (subclinical patients; scans performed before symptom onset).
- Group 2 (scans performed ≤1 week after symptom onset).
- Group 3 (> 1 week to 2 weeks).
- Group 4 (> 2 weeks to 3 weeks).
The characteristics of the images and their distribution were analyzed and compared in the four groups.
Results
Patients were assigned to groups based on the time between the onset of symptoms and the first CT scan: 15 (19%) patients were assigned to group 1, 21 (26%) to group 2, 30 (37%) to group 3, and 15 (19%) to group 4.
The average age was 49.5 years, and there was no gender difference. No significant differences in age or sex distribution were identified between the groups.
The most common symptoms at onset were fever (73% of patients) and dry cough (59%).
Other nonspecific symptoms included dizziness (2%), diarrhea (4%), vomiting (5%), headache (6%), and generalized weakness (9%). Between groups 2–4 (symptomatic patients), no significant differences in clinical parameters were found.
Patients in group 1 had significantly lower mean concentrations of C-reactive protein (6.9 mg/L) and aspartate aminotransferase (30.2 U/L) than patients in the rest of the groups.
All patients had abnormal CT imaging features. Although all lung segments may be involved, there was a slight predilection for the right lower lobe .
The mean number of segments involved among all groups was 10.5, with significantly more segments involved in groups 2–4 (symptomatic patients) than group 1 (asymptomatic patients). Group 3 had the highest mean number of segments involved.
Sixty-four (79%) patients had bilateral lung involvement, 44 (54%) showed peripheral distribution, and 36 (44%) showed diffuse distribution of abnormalities on CT (Figure 1).
The most common patterns observed on chest CT were ground glass opacity (65% of patients, Fig. 1 A), as well as poorly defined margins (81%), smooth or irregular interlobular septal thickening (35%, Fig. . 1 A), air bronchogram (47%, Fig. 1 A, D), cobblestone pattern (10%, Fig. 1 B) and thickening of the adjacent pleura (32%).
The less frequent findings on CT were nodules, cystic changes (10%, Fig. 1 C), bronchiectasis, pleural effusion (5%, Fig. 2 D), and lymphadenopathy. No tree pattern in budding, masses, cavitation, and calcifications were observed in this case series.
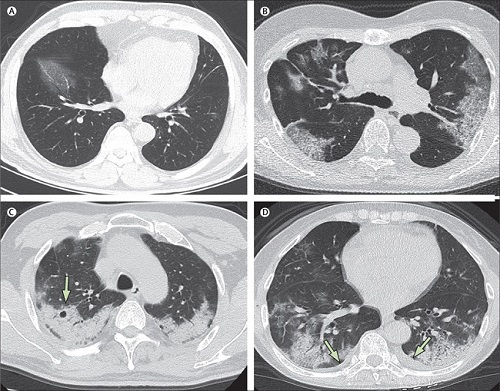
Figure 1
The typical pattern of CT imaging features of preclinical patients (group 1) comprised unilateral, multifocal, and ground-glass opacification.
In group 2 (first week after symptom onset), the lesions rapidly evolved to become bilateral and diffuse, but remained predominantly ground-glass opacity-like. Pleural effusion and lymphadenopathy were detected at this stage.
In group 3 (second week after symptom onset), as the disease progressed, the ground-glass opacity pattern remained the predominant finding on CT; however, consolidation patterns were also observed.
In group 4 (third week after symptom onset), ground-glass opacities and reticular patterns were the predominant imaging pattern. Bronchiectasis, thickening of the adjacent pleura, effusions, and lymphadenopathy may also be seen at this stage.
By February 8, 2020, 62 (77%) patients had been discharged, with a mean interval between symptom onset and discharge of 23.2 days; Sixteen (20%) patients were still in hospital, and three (4%) patients had died (on days 12, 14 and 30, after hospital admission due to ARDS).
Patient 1, who died on day 12 after admission, was a 60-year-old man with chronic lung disease (tuberculosis). Computed tomography obtained from this patient on day 8 after symptom onset showed extensive ground-glass opacities in both lungs, giving a white lung appearance (Fig. 2).
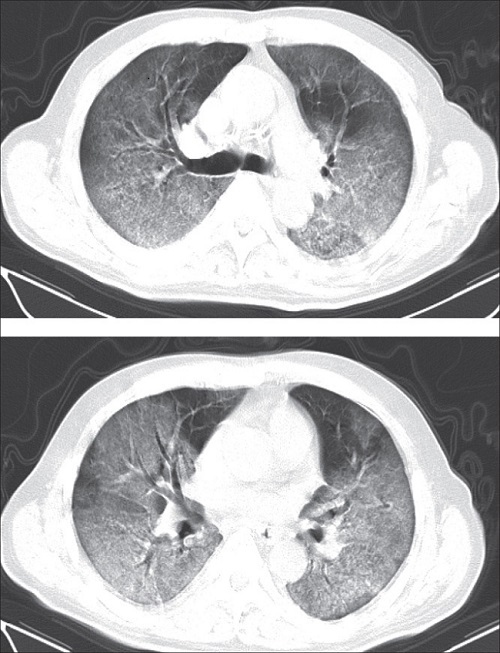
Figure 2
Patient 2 who died was a 73-year-old man who had had type 2 diabetes for several years, and showed progressive radiographic deterioration on CT scans taken on days 3, 7, and 11 after symptom onset. Patient 3, who died on day 30 after admission, was a 77-year-old man with hypertension, cardiovascular disease, and cerebrovascular disease.
A CT scan showed mild pneumonia on day 5 after symptom onset in this patient (Fig. 3 A), and two follow-up CT scans 10 days and 15 days later revealed rapid progression of lung lesions with bilateral pleural effusions. (fig. 3 B, C).
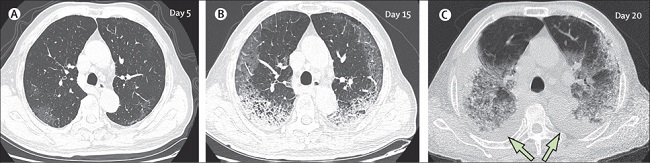
Figure 3
Follow-up CT images were obtained from 57 (70%) patients.
Four patterns of evolution were observed throughout the series of CT scans among these 57 patients: initial progression to maximum level, followed by radiographic improvement (type 1), observed in 26 (46%) patients (Fig. 4), of of which 24 (92%) patients were discharged from the hospital; radiographic deterioration (type 2), seen in 18 (32%) patients (fig. 3), of whom two (11%) died (patients 2 and 3); radiographic improvement (type 3), observed in eight (14%) patients, of whom five (63%) were discharged from the hospital; and unchanged radiographic appearance (type 4), seen in five (9%) patients, all of whom were still in the hospital on the cut-off date (February 8).
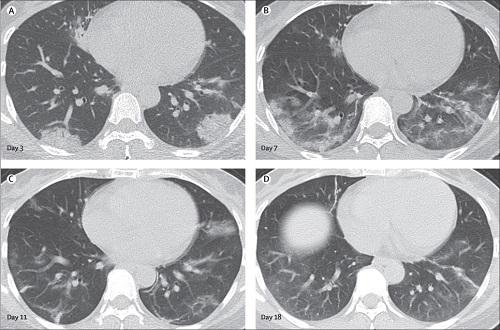
Figure 4
Discussion
The new coronavirus SARS-CoV-2 is the seventh member of the Coronaviridae family known to infect humans. The mortality rate of COVID-19 so far is lower than that of the SARS or MERS coronavirus diseases; However, SARS-CoV-2 is highly infectious and could be a significant health threat.
In this study, predisposing conditions for COVID-19 pneumonia tended to be old age and medical comorbidities (such as chronic lung disease, diabetes, and other chronic diseases), similar to previous viral infections such as H7N9 influenza. There was no obvious predilection for men or women in this cohort.
However, the authors mention another study, which reported that 30 (73%) of 41 infected patients were men. This discrepancy could be due to differences in demographic characteristics and small cohorts.
By February 8, 2020, three patients in the study had died, representing a mortality rate of about 4%.
All of the deaths occurred in men over 60 who had underlying conditions, consistent with previous reports. Therefore, old age, male sex, and the presence of comorbidities may be risk factors for a poor prognosis.
Fever, cough, and dyspnea were the most common symptoms in patients with COVID-19 pneumonia, which is consistent with the manifestation of lower respiratory tract infections. In contrast, upper respiratory tract symptoms were less common in these patients, indicating that the cells targeted by the virus could be located in the lower airway.
15 cases of asymptomatic infection were discovered on the basis of abnormal lung findings on CT scans, suggesting that chest CT scans or serum antibody testing should be performed in high-risk asymptomatic individuals with a history of exposure to patients with COVID-19 pneumonia to facilitate early identification of the disease.
The mean number of lung segments involved in this cohort was 10.5, with the right lower lobes most commonly affected. This finding could be due to the anatomical structure of the trachea and bronchi: since the right bronchus is short and straight, the causative virus could tend to favor this location.
The extent of disease on CT scans showed a marked increase from the subclinical period to the first and second week after symptom onset, then gradually decreased in the third week. Therefore, these findings indicate that the radiological evolution of COVID-19 pneumonia is consistent with the clinical course of the disease.
Most patients in the cohort showed bilateral pulmonary involvement , with lesions located mainly peripherally and subpleurally with diffuse distribution. The predominant pattern was ground glass opacity , with poorly defined margins, air bronchograms, smooth or irregular interlobular or septal thickening, and thickening of the adjacent pleura.
These imaging features are non-specific and bear some resemblance to those of SARS-CoV and MERS-CoV infections.
However, unlike SARS-CoV infections, some patients in our study presented with pleural effusion, lymphadenopathy, and round cystic changes on CT. Previous studies demonstrated that the presence of pleural effusion in patients infected with MERS-CoV or H5N1 avian influenza was a poor prognostic indicator. Similarly, in the third patient who died in the study, a follow-up CT scan showed that he had developed bilateral pleural effusion.
However, none of the CT features of COVID-19 appear to be specific or diagnostic, and COVID-19 pneumonia shares CT features with other noninfectious conditions that present as subpleural airspace disease.
The typical pattern of CT images in subclinical patients (group 1) was unilateral, multifocal, predominantly ground-glass opacities.
In the first week after symptom onset (group 2), the lesions rapidly progressed to bilateral diffuse disease, with a relative decrease in the frequency of ground-glass opacities and a transition to consolidation and the development of mixed patterns. Pleural effusion and lymphadenopathy were also detected in group 2.
Subsequently, ground-glass opacities continued to decrease in frequency during the second week after symptom onset (group 3), while consolidation became the second most common pattern.
It was also observed that a reticular pattern associated with bronchiectasis and irregular interlobular or septal thickening progressively increases from the second week. These findings indicated the appearance of interstitial changes, suggesting the development of fibrosis.
As the disease progressed in the third week after symptom onset, consolidation and mixed patterns became more common, while ground-glass opacities decreased further.
Bronchiectasis, thickening of the adjacent pleura, and pleural effusion mainly appeared at this stage.
Follow-up CT showed progression or improvement of lung lesions during treatment, which sensitively reflects the therapeutic effects, and these changes could be related to the results in these patients. The most common pattern of progression across the series of CT scans in this study was initial progression to a maximum level, followed by radiographic improvement (type 1), and the majority of these patients were subsequently discharged.
Furthermore, most patients who showed a pattern of radiographic improvement on multiple scans (type 3) were discharged from the hospital. Therefore, a type 1 or type 3 disease course could be associated with favorable outcomes. On the other hand, progressive radiographic deterioration despite medical treatment appears to be associated with a poor prognosis.
Conclusions
|
















